Transcribed Image Text from this Question
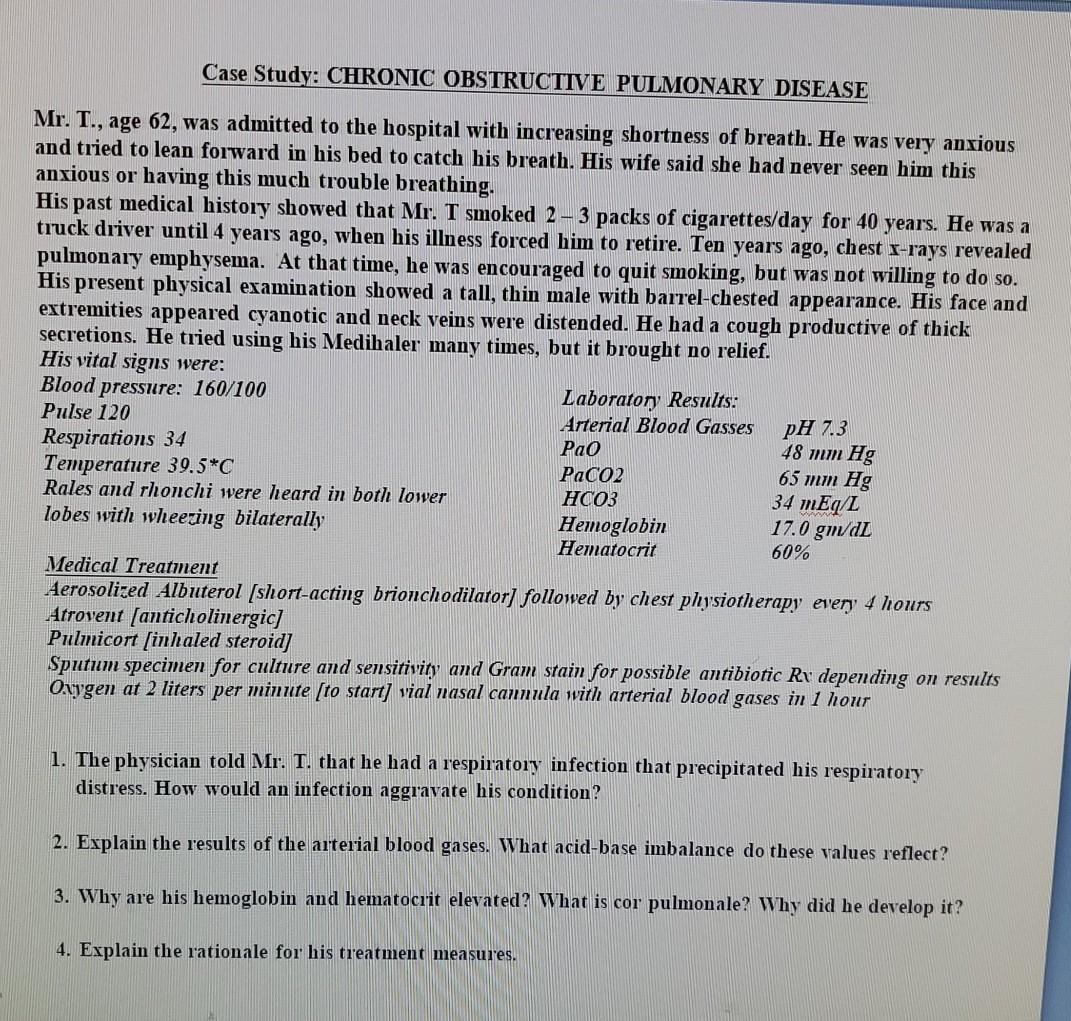
Case Study: CHRONIC OBSTRUCTIVE PULMONARY DISEASE Mr. T., age 62, was admitted to the hospital with increasing shortness of breath. He was very anxious and tried to lean forward in his bed to catch his breath. His wife said she had never seen him this anxious or having this much trouble breathing. His past medical history showed that Mr. T smoked 2- 3 packs of cigarettes/day for 40 years. He was a truck driver until 4 years ago, when his illness forced him to retire. Ten years ago, chest x-rays revealed pulmonary emphysema. At that time, he was encouraged to quit smoking, but was not willing to do so. His present physical examination showed a tall, thin male with barrel-chested appearance. His face and extremities appeared cyanotic and neck veins were distended. He had a cough productive of thick secretions. He tried using his Medihaler many times, but it brought no relief. His vital signs were: Blood pressure: 160/100 Laboratory Results: Pulse 120 Arterial Blood Gasses Respirations 34 Pao 48 mm Hg Temperature 39.5*C PaCo2 65 mm Hg Rales and rhonchi were heard in both lower HCO3 34 mEq/L lobes with wheezing bilaterally Hemoglobin 17.0 gm/dL Hematocrit 60% Medical Treatment Aerosolized Albuterol (short-acting brionchodilator] followed by chest physiotherapy every 4 hours Atrovent (anticholinergic] Pulmicort (inhaled steroid] Sputum specimen for culture and sensitivity and Gram stain for possible antibiotic Rr depending on results Oxygen at 2 liters per minute (to start] vial nasal cannula with arterial blood gases in 1 hour pH 7.3 1. The physician told Mr. 1. that he had a respiratory infection that precipitated his respiratory distress. How would an infection aggravate his condition? 2. Explain the results of the arterial blood gases. What acid-base imbalance do these values reflect? 3. Why are his hemoglobin and hematocrit elevated? What is cor pulmonale? Why did he develop it? 4. Explain the rationale for his treatment measures.
(Visited 2 times, 1 visits today)