Transcribed Image Text from this Question
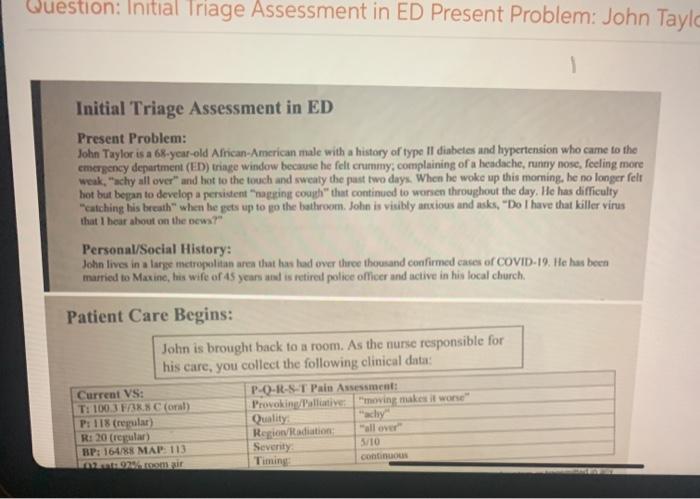
Question: Initial Triage Assessment in ED Present Problem: John Taylo Initial Triage Assessment in ED Present Problem: John Taylor is a 68-year-old African-American male with a history of type Il diabetes and hypertension who came to the emergency department (ED) triage window because he felt crummy, complaining of a headache, runny nose, feeling more weak, “achy all over” and hot to the touch and sweaty the past two days. When he woke up this morning, he no longer felt hot but boppan to develop a persistent “agging couch” that continued to wonien throughout the day. He has difficulty catching his breath” when he gets up to go the bathroom. John is visibly anxious and asks, “Do I have that killer virus that I hear about on the news?” Personal/Social History: John lives in a large metropolitan area that has had over three thousand confirmed cases of COVID-19. He has been married to Maxine, his wife of 15 years and is retired police officer and active in his local church Patient Care Begins: John is brought back to a room. As the nurse responsible for his care, you collect the following clinical data: Current VS: P-O-R-S-T Pain Assessment: T: 100.3 FN Coral) Provoking/Pallative moving makes it worse” P: 118 (regular) Quality R: 20 (regular) Region Radiation all over BP: 164/88 MAP: 113 Severity 5/10 2. continuous
(Visited 4 times, 1 visits today)



