Transcribed Image Text from this Question
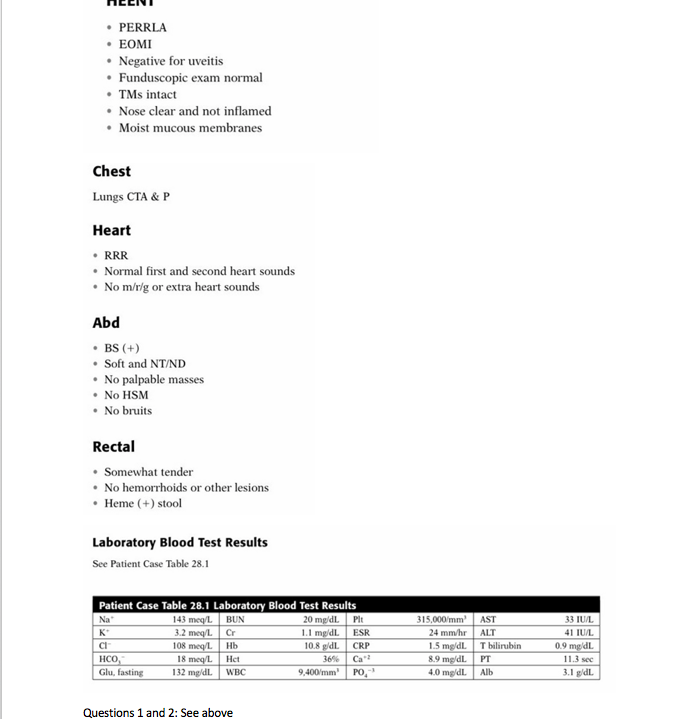
X.P. is a 24-year-old man, who presents to the urgent care clinic with complaints of rectal bleeding and weakness. Five days ago he noticed bright red blood in his stools. Furthermore, daily bowel movements have increased to five or six with significant diarrhea. He states that urges to move his bowels have rapid onset, but there has been no incontinence. He has been weak for approximately 2′ days. He has not traveled outside of the city, been hospitalized, or received antibiotics recently. Patient Case Question 1. What is the relevance of the last sentence directly above? PMH • Chronic sinus infections since age 15 • Ventricular septal defect at birth, surgically repaired at age 1 year FH Strong positive family history of autoimmune disease on maternal side • Mother has SLE • Maternal grandmother (deceased) had Graves disease • Aunt has myasthenia gravis Patient Case Question 2. What is the significance of the patient’s family history? SH • College graduate • Recently discharged after 3 years of active military service in Afghanistan • Currently employed as user consultant in information technology division at local com- munity college • Social alcohol use only • Denies tobacco and IV drug use ROS • Negative for lightheadedness and feeling faint with standing • Negative for nausea, vomiting, visual changes or eye pain, abdominal distension with gas, and joint pain • Positive for occasional malaise, mild abdominal cramps, loss of appetite, and weight loss of 4 lbs during the past month Meds None All NKDA PE and Lab Tests Gen A & O, pleasant, young, white male in NAD; skin color is pale VS BP (sitting, left arm) 120/75, P 93 bpm, RR 20/min, T 99.4°F, Sao, 95% on RA, Wt 161 lbs (usual weight 165 lbs), Ht 5’10” Skin • Warm and dry with satisfactory turgor • Positive for pallor • No rashes or other lesions • PERRLA • EOMI • Negative for uveitis • Funduscopic exam normal • TMs intact • Nose clear and not inflamed • Moist mucous membranes Chest Lungs CTA & P Heart • RRR • Normal first and second heart sounds • No m/r/g or extra heart sounds Abd • BS(+) • Soft and NT/ND • No palpable masses • No HSM • No bruits Rectal Somewhat tender No hemorrhoids or other lesions • Heme (+) stool Laboratory Blood Test Results See Patient Case Table 28.1 Patient Case Table 28.1 Laboratory Blood Test Results Na 143 meq/L BUN 20 mg/dL. Plt K 3.2 meq/L Cr 1.1 mg/dl. ESR CI 108 megl 10.8 gdL CRP HCO, 18 meq/L 36% Glu, fasting 132 mg/dL. 9,400/mm Hb Het WBC 315,000/mm 24 mm/hr 1.5 mg/dl. 8.9 mg/dl. 4.0 mg/dl. AST ALT Tbilirubin PT Alb 33 IU/L 41 IU/L 0.9 mg/dl. 11.3 sec 3.1 gldl Can? PO, Questions 1 and 2: See above 3. What is a reasonable explanation for pallor in this patient? 4. What does satisfactory turgor and moist mucous membranes indicate? 5. Identify eight abnormal laboratory blood test values and provide a brief pathophysiologic explanation for each of them. 6. Does the patient have signs of liver disease?
(Visited 3 times, 1 visits today)