Transcribed Image Text from this Question
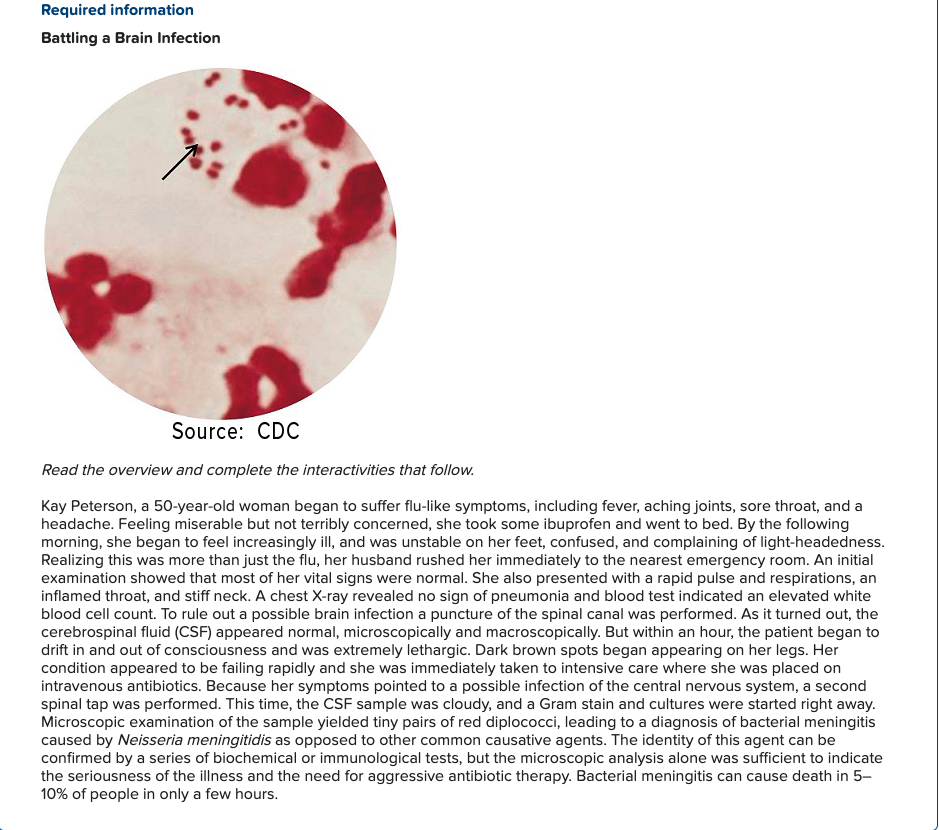
Required information Battling a Brain Infection Source: CDC Read the overview and complete the interactivities that follow. Kay Peterson, a 50-year-old woman began to suffer flu-like symptoms, including fever, aching joints, sore throat, and a headache. Feeling miserable but not terribly concerned, she took some ibuprofen and went to bed. By the following morning, she began to feel increasingly ill, and was unstable on her feet, confused, and complaining of light-headedness. Realizing this was more than just the flu, her husband rushed her immediately to the nearest emergency room. An initial examination showed that most of her vital signs were normal. She also presented with a rapid pulse and respirations, an inflamed throat, and stiff neck. A chest X-ray revealed no sign of pneumonia and blood test indicated an elevated white blood cell count. To rule out a possible brain infection a puncture of the spinal canal was performed. As it turned out, the cerebrospinal fluid (CSF) appeared normal, microscopically and macroscopically. But within an hour, the patient began to drift in and out of consciousness and was extremely lethargic. Dark brown spots began appearing on her legs. Her condition appeared to be failing rapidly and she was immediately taken to intensive care where she was placed on intravenous antibiotics. Because her symptoms pointed to a possible infection of the central nervous system, a second spinal tap was performed. This time, the CSF sample was cloudy, and a Gram stain and cultures were started right away. Microscopic examination of the sample yielded tiny pairs of red diplococci, leading to a diagnosis of bacterial meningitis caused by Neisseria meningitidis as opposed to other common causative agents. The identity of this agent can be confirmed by a series of biochemical or immunological tests, but the microscopic analysis alone was sufficient to indicate the seriousness of the illness and the need for aggressive antibiotic therapy. Bacterial meningitis can cause death in 5- 10% of people in only a few hours. The Gram Stain and Other Diagnostic Methods Because of the severity of bacterial meningitis, it is imperative that diagnosis is made quickly and correctly. Locate this journal reference using an online database to read about limitations in diagnostic approaches to patients with suspected meningitis: Huynh W, Lahoria R, Beran RG, Cordato D. “Meningococcal meningitis and a negative cerebrospinal fluid: case report and its medicolegal implications.” Emerg Med Australas. 2007 Dec; 19(6):553-5. doi: 10.1111/j.1742-6723.2007.01032.x Read the article thoroughly, and then discuss the following. 1. What has been the traditional purpose of CSF testing on patients that present with possible meningitis? What shortcoming does CSF testing have, and what might be the ramifications of its use for this traditional purpose? 2. Compare and contrast the patient in the introduction with the patient in this journal article. 3. Conducting further research, explain the basis for the brown spots on the case patient and the purpuric rash on the patient in this article. What does this sign indicate to the physician? 4. Culture showed positive in both cases for bacterial meningitis. Are other tests necessary for diagnosis, and if so, why? 5. According to the authors of this journal article, what is sufficient to prompt the use of antibiotic therapy in a case of suspected meningitis? 6. Conducting additional research, write a brief description of two other major bacterial pathogens that can cause meningitis.
(Visited 2 times, 1 visits today)