Transcribed Image Text from this Question
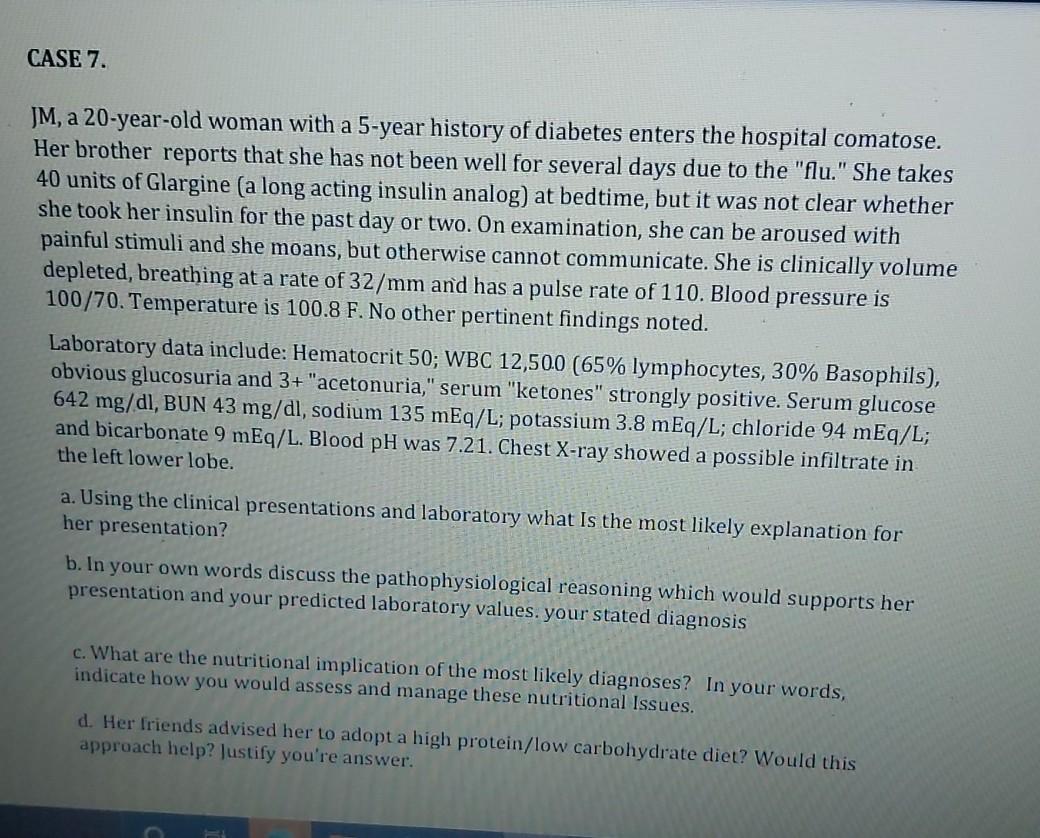
CASE 7. JM, a 20-year-old woman with a 5-year history of diabetes enters the hospital comatose. Her brother reports that she has not been well for several days due to the “flu.” She takes 40 units of Glargine (a long acting insulin analog) at bedtime, but it was not clear whether she took her insulin for the past day or two. On examination, she can be aroused with painful stimuli and she moans, but otherwise cannot communicate. She is clinically volume depleted, breathing at a rate of 32/mm and has a pulse rate of 110. Blood pressure is 100/70. Temperature is 100.8 F. No other pertinent findings noted. Laboratory data include: Hematocrit 50; WBC 12,500 (65% lymphocytes, 30% Basophils), obvious glucosuria and 3+ “acetonuria,” serum “ketones” strongly positive. Serum glucose 642 mg/dl, BUN 43 mg/dl, sodium 135 mEq/L; potassium 3.8 mEq/L; chloride 94 mEq/L; and bicarbonate 9 mEq/L. Blood pH was 7.21. Chest X-ray showed a possible infiltrate in the left lower lobe. a. Using the clinical presentations and laboratory what is the most likely explanation for her presentation? b. In your own words discuss the pathophysiological reasoning which would supports her presentation and your predicted laboratory values. your stated diagnosis c. What are the nutritional implication of the most likely diagnoses? In your words, indicate how you would assess and manage these nutritional Issues. d. Her friends advised her to adopt a high protein/low carbohydrate diet? Would this approach help? Justify you’re answer.
(Visited 2 times, 1 visits today)