Transcribed Image Text from this Question
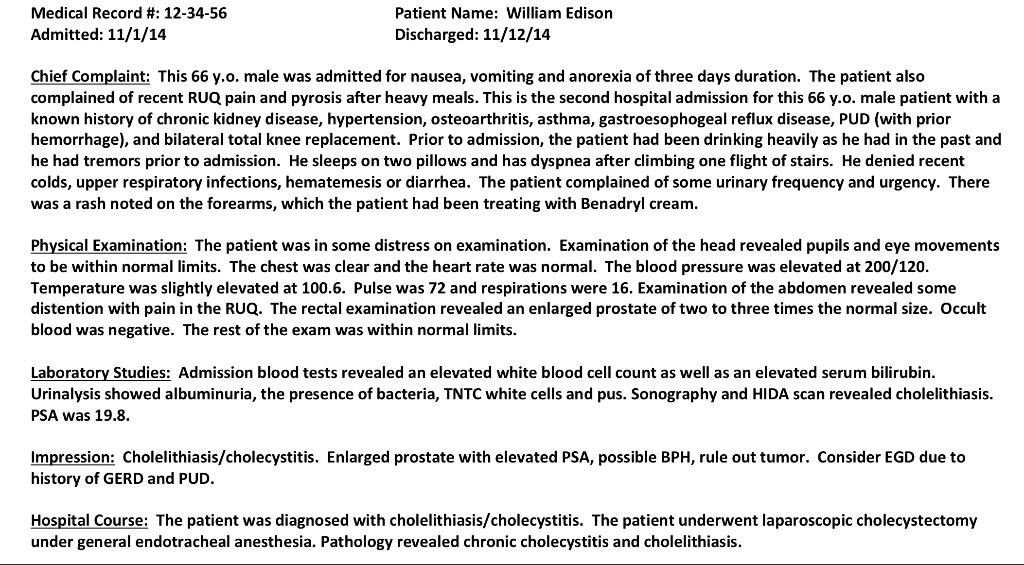
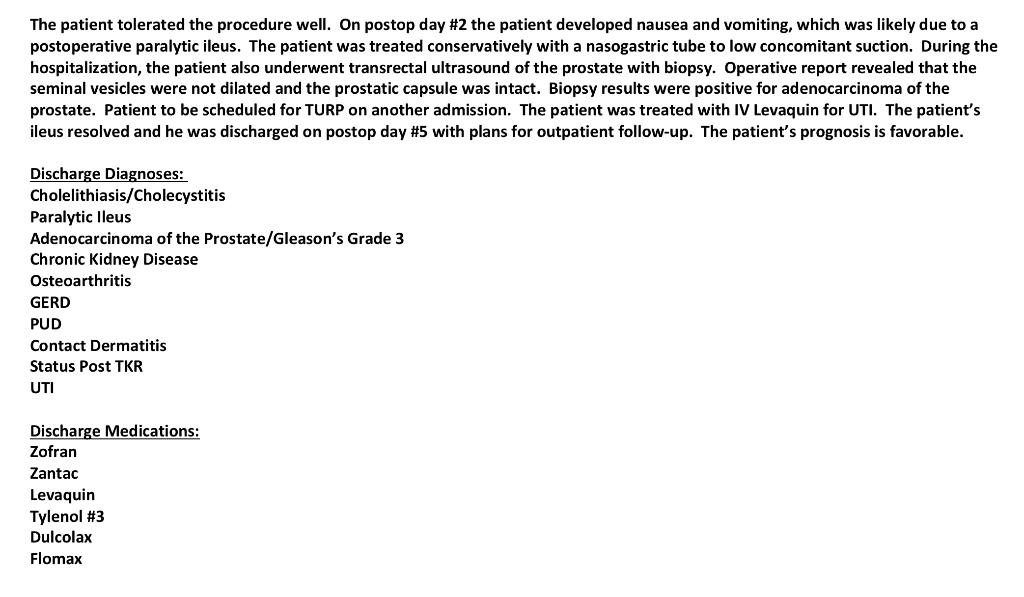
Medical Record #: 12-34-56 Admitted: 11/1/14 Patient Name: William Edison Discharged: 11/12/14 Chief Complaint: This 66 y.o. male was admitted for nausea, vomiting and anorexia of three days duration. The patient also complained of recent RUQ pain and pyrosis after heavy meals. This is the second hospital admission for this 66 y.o. male patient with a known history of chronic kidney disease, hypertension, osteoarthritis, asthma, gastroesophogeal reflux disease, PUD (with prior hemorrhage), and bilateral total knee replacement. Prior to admission, the patient had been drinking heavily as he had in the past and he had tremors prior to admission. He sleeps on two pillows and has dyspnea after climbing one flight of stairs. He denied recent colds, upper respiratory infections, hematemesis or diarrhea. The patient complained of some urinary frequency and urgency. There was a rash noted on the forearms, which the patient had been treating with Benadryl cream. Physical Examination: The patient was in some distress on examination. Examination of the head revealed pupils and eye movements to be within normal limits. The chest was clear and the heart rate was normal. The blood pressure was elevated at 200/120. Temperature was slightly elevated at 100.6. Pulse was 72 and respirations were 16. Examination of the abdomen revealed some distention with pain in the RUQ. The rectal examination revealed an enlarged prostate of two to three times the normal size. Occult blood was negative. The rest of the exam was within normal limits. Laboratory Studies: Admission blood tests revealed an elevated white blood cell count as well as an elevated serum bilirubin. Urinalysis showed albuminuria, the presence of bacteria, TNTC white cells and pus. Sonography and HIDA scan revealed cholelithiasis. PSA was 19.8. Impression: Cholelithiasis/cholecystitis. Enlarged prostate with elevated PSA, possible BPH, rule out tumor. Consider EGD due to history of GERD and PUD. Hospital Course: The patient was diagnosed with cholelithiasis/cholecystitis. The patient underwent laparoscopic cholecystectomy under general endotracheal anesthesia. Pathology revealed chronic cholecystitis and cholelithiasis. The patient tolerated the procedure well. On postop day #2 the patient developed nausea and vomiting, which was likely due to a postoperative paralytic ileus. The patient was treated conservatively with a nasogastric tube to low concomitant suction. During the hospitalization, the patient also underwent transrectal ultrasound of the prostate with biopsy. Operative report revealed that the seminal vesicles were not dilated and the prostatic capsule was intact. Biopsy results were positive for adenocarcinoma of the prostate. Patient to be scheduled for TURP on another admission. The patient was treated with IV Levaquin for UTI. The patient’s ileus resolved and he was discharged on postop day #5 with plans for outpatient follow-up. The patient’s prognosis is favorable. Discharge Diagnoses: Cholelithiasis/Cholecystitis Paralytic lleus Adenocarcinoma of the Prostate/Gleason’s Grade 3 Chronic Kidney Disease Osteoarthritis GERD PUD Contact Dermatitis Status Post TKR UTI Discharge Medications: Zofran Zantac Levaquin Tylenol #3 Dulcolax Flomax 13. The patient developed a paralytic ileus. Describe this condition and list one reason why it can occur following surgery. 14. The seminal vesicles were noted to be “non-dilated. What is the function of the seminal vesicles? 15. The patient was said to have possible BPH. Describe this condition.
(Visited 4 times, 1 visits today)