Transcribed Image Text from this Question
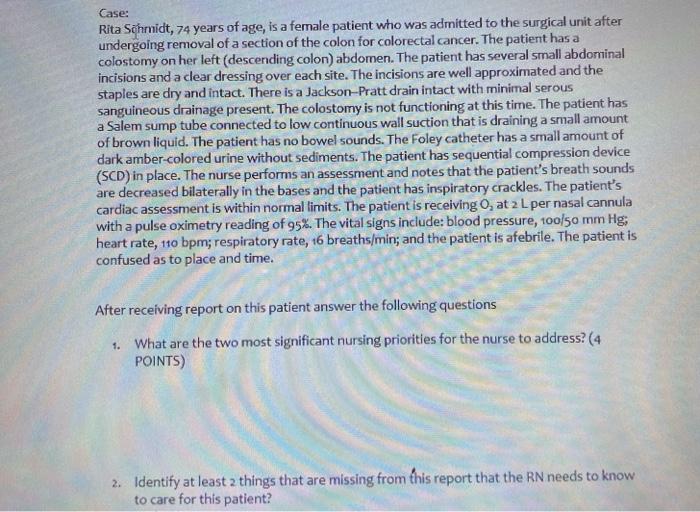
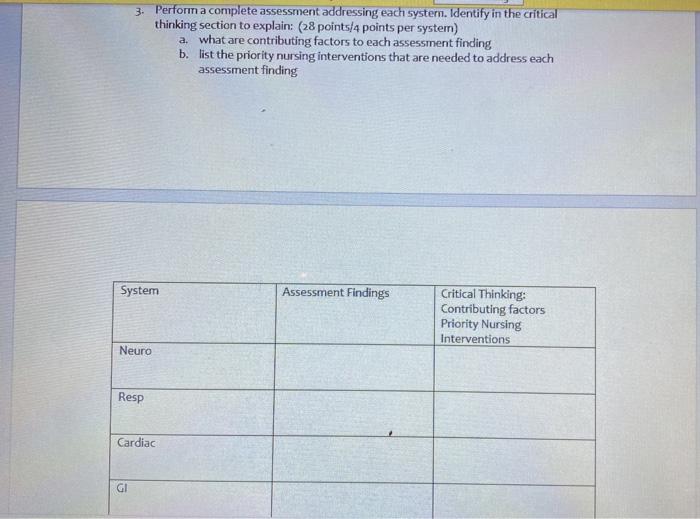
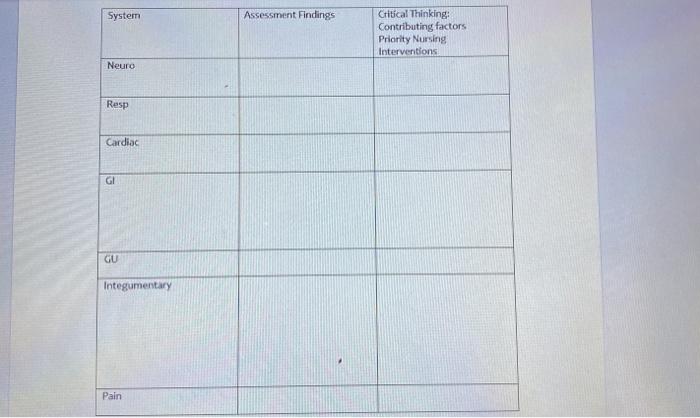
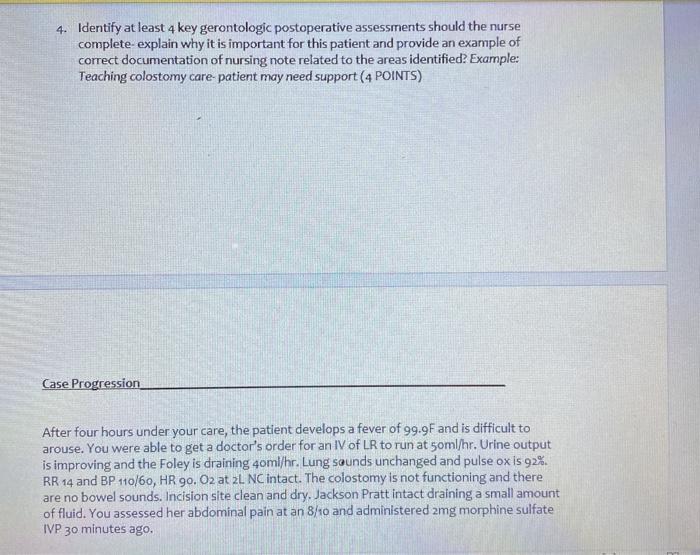
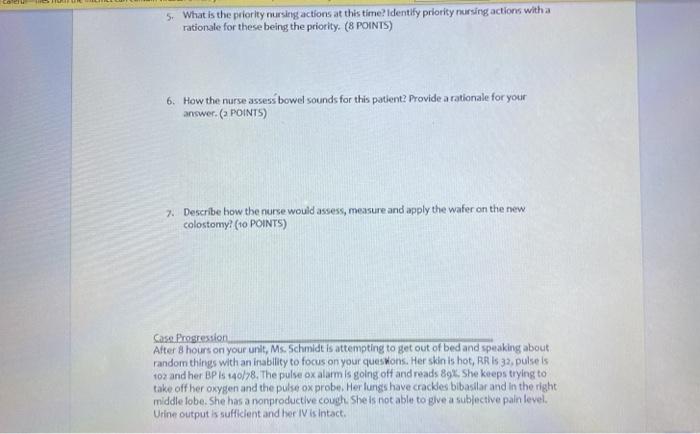
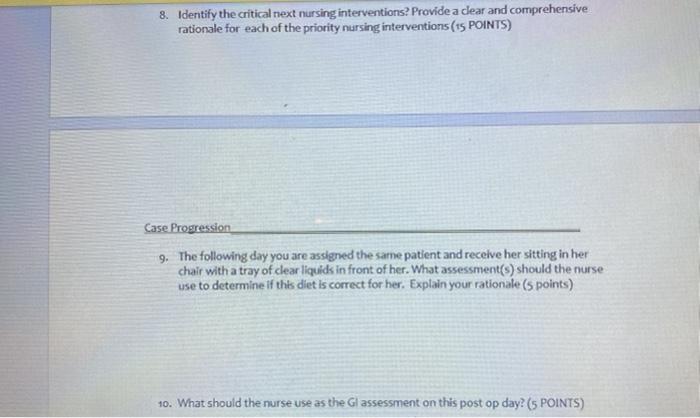
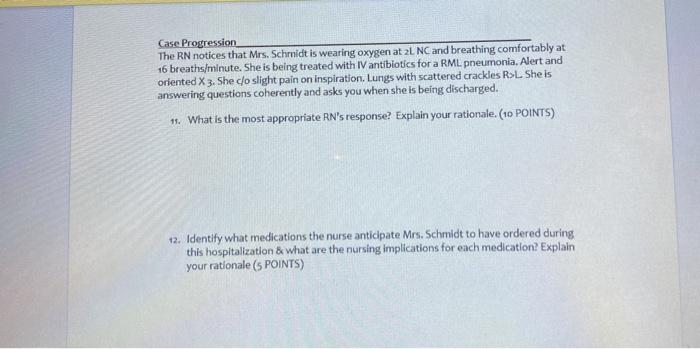
Case: Rita Schmidt, 74 years of age, is a female patient who was admitted to the surgical unit after undergoing removal of a section of the colon for colorectal cancer. The patient has a colostomy on her left (descending colon) abdomen. The patient has several small abdominal incisions and a clear dressing over each site. The incisions are well approximated and the staples are dry and intact. There is a Jackson-Pratt drain intact with minimal serous sanguineous drainage present. The colostomy is not functioning at this time. The patient has a Salem sump tube connected to low continuous wall suction that is draining a small amount of brown liquid. The patient has no bowel sounds. The Foley catheter has a small amount of dark amber-colored urine without sediments. The patient has sequential compression device (SCD) in place. The nurse performs an assessment and notes that the patient’s breath sounds are decreased bilaterally in the bases and the patient has inspiratory crackles. The patient’s cardiac assessment is within normal limits. The patient is receiving O, at 2 L per nasal cannula with a pulse oximetry reading of 95%. The vital signs include: blood pressure, 100/50 mm Hg: heart rate, 110 bpm; respiratory rate, 16 breaths/min; and the patient is afebrile. The patient is confused as to place and time. After receiving report on this patient answer the following questions 1. What are the two most significant nursing priorities for the nurse to address? (4 POINTS) 2. Identify at least 2 things that are missing from this report that the RN needs to know to care for this patient? 3. Perform a complete assessment addressing each system. Identify in the critical thinking section to explain: (28 points/4 points per system) a. what are contributing factors to each assessment finding b. list the priority nursing interventions that are needed to address each assessment finding System Assessment Findings Critical Thinking: Contributing factors Priority Nursing Interventions Neuro Resp Cardiac GI System Assessment Findings Critical Thinking: Contributing factors Priority Nursing Interventions Neuro Resp Cardiac GI GU Integumentary Pain 4. Identify at least 4 key gerontologic postoperative assessments should the nurse complete-explain why it is important for this patient and provide an example of correct documentation of nursing note related to the areas identified? Examples Teaching colostomy care patient may need support (4 POINTS) Case Progression After four hours under your care, the patient develops a fever of 99.9F and is difficult to arouse. You were able to get a doctor’s order for an IV of LR to run at soml/hr. Urine output is improving and the Foley is draining 4oml/hr. Lung sounds unchanged and pulse ox is 92%. RR 14 and BP 110/60, HR 90. O2 at 2L NC intact. The colostomy is not functioning and there are no bowel sounds. Incision site clean and dry, Jackson Pratt intact draining a small amount of fluid. You assessed her abdominal pain at an 8/10 and administered amg morphine sulfate TVP 30 minutes ago 5. What is the priority nursing actions at this time? Identify priority nursing actions with a rationale for these being the priority. (8 POINTS) 6. How the nurse assess bowel sounds for this patient? Provide a rationale for your answer. (POINTS) 7. Describe how the nurse would assess, measure and apply the wafer on the new colostomy? (10 POINTS) Case Progression After 8 hours on your unit, Ms. Schmidt is attempting to get out of bed and speaking about random things with an inability to focus on your queswons. Her skin is hot, RR IS 32, pulseis 102 and her BP is 140/78. The pulse oxalarm is going off and reads 89%. She keeps trying to take off her oxygen and the pulse ox probe. Her lungs have crackdes bibasilar and in the right middle lobe. She has a nonproductive cough. She is not able to give a subjective pain level. Urine output is sufficient and her IV is intact. 8. Identify the critical next nursing interventions? Provide a dear and comprehensive rationale for each of the priority nursing interventions ( 15 POINTS) Case Progression 9. The following day you are assigned the same patient and receive her sitting in her chair with a tray of clear liquids in front of her. What assessment(s) should the nurse use to determine if this diet is correct for her. Explain your rationale (5 points) 10. What should the nurse use as the Gl assessment on this post op day? (5 POINTS) Case Progression The RN notices that Mrs. Schmidt is wearing oxygen at 2L NC and breathing comfortably at 16 breaths/minute. She is being treated with IV antibiotics for a RML. pneumonia. Alert and oriented X 3. She do slight pain on inspiration. Lungs with scattered crackles RL She is answering questions coherently and asks you when she is being discharged. 11. What is the most appropriate RN’s response? Explain your rationale. (10 POINTS) 12. Identify what medications the nurse anticipate Mrs. Schmidt to have ordered during this hospitalization & what are the nursing implications for each medication? Explain your rationale (S POINTS)
(Visited 10 times, 1 visits today)



