Transcribed Image Text from this Question
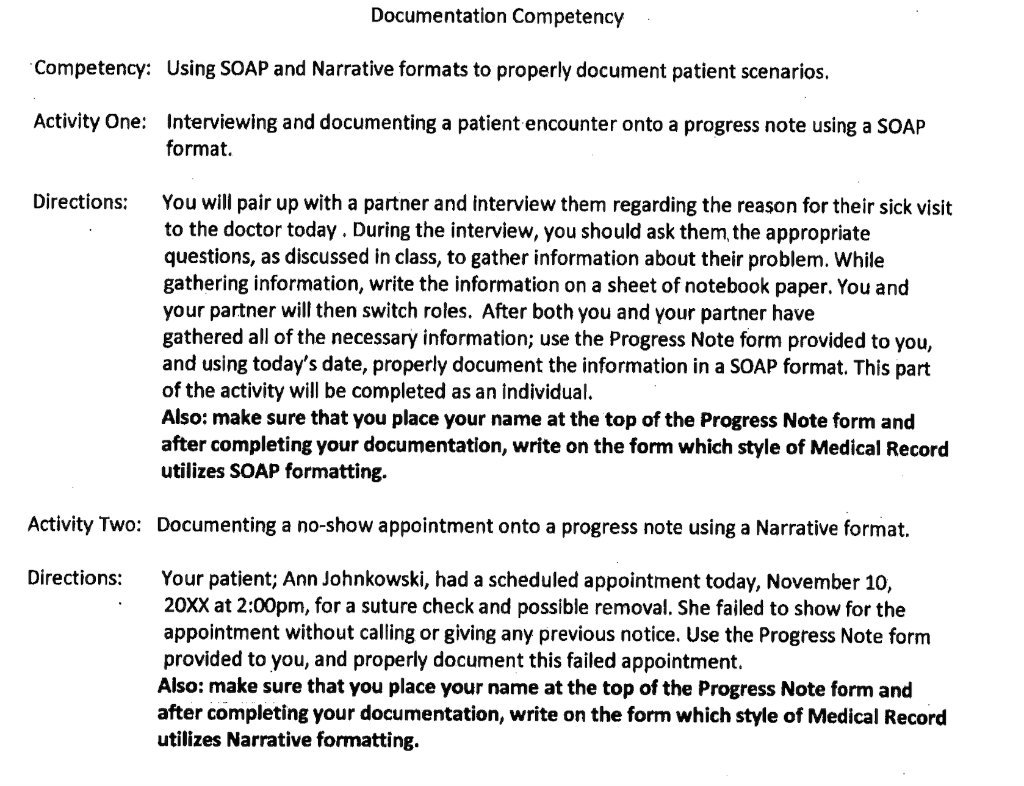
Documentation Competency Competency: Using SOAP and Narrative formats to properly document patient scenarios. Activity One: Interviewing and documenting a patient encounter onto a progress note using a SOAP format. Directions: You will pair up with a partner and interview them regarding the reason for their sick visit to the doctor today. During the interview, you should ask them the appropriate questions, as discussed in class, to gather information about their problem. While gathering information, write the information on a sheet of notebook paper. You and your partner will then switch roles. After both you and your partner have gathered all of the necessary information; use the Progress Note form provided to you, and using today’s date, properly document the information in a SOAP format. This part of the activity will be completed as an individual. Also: make sure that you place your name at the top of the Progress Note form and after completing your documentation, write on the form which style of Medical Record utilizes SOAP formatting. Activity Two: Documenting a no-show appointment onto a progress note using a Narrative format. Directions: Your patient; Ann Johnkowski, had a scheduled appointment today, November 10, 20XX at 2:00pm, for a suture check and possible removal. She failed to show for the appointment without calling or giving any previous notice. Use the Progress Note form provided to you, and properly document this failed appointment. Also: make sure that you place your name at the top of the Progress Note form and after completing your documentation, write on the form which style of Medical Record utilizes Narrative formatting.
(Visited 4 times, 1 visits today)