Question: A 74 year old woman has an appointment at the clinic where you work. She is complaining of aching…
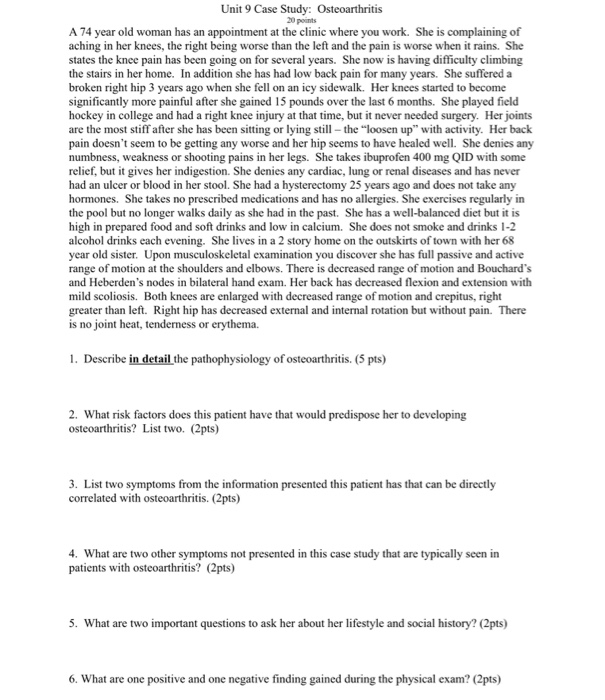
Show transcribed image text A 74 year old woman has an appointment at the clinic where you work. She is complaining of aching in her knees, the right being worse than the left and the pain is worse when it rains. She states the knee pain has been going on for several years. She now is having difficulty climbing the stairs in her home. In addition she has had low back pain for many years. She suffered a broken right hip 3 years ago when she fell on an icy sidewalk. Her knees started to become significantly more painful after she gained 15 pounds over the last 6 months. She played field hockey in college and had a right knee injury at that time, but it never needed surgery. Her joints are the most stiff after she has been sitting or lying still – the "loosen up" with activity. Her back pain doesn't seem to be getting any worse and her hip seems to have healed well. She denies any numbness, weakness or shooting pains in her legs. She takes ibuprofen 400 mg QID with some relief, but it gives her indigestion. She denies any cardiac, lung or renal diseases and has never had an ulcer or blood in her stool. She had a hysterectomy 25 years ago and does not take any hormones. She takes no prescribed medications and has no allergies. She exercises regularly in the pool but no longer walks daily as she had in the past. She has a well-balanced diet but it is high in prepared food and soft drinks and low in calcium. She does not smoke and drinks 1-2 alcohol drinks each evening. She lives in a 2 story home on the outskirts of town with her 68 year old sister. Upon musculoskeletal examination you discover she has full passive and active range of motion at the shoulders and elbows. There is decreased range of motion and Bouchard's and Heberden's nodes in bilateral hand exam. Her back has decreased flexion and extension with mild scoliosis. Both knees are enlarged with decreased range of motion and crepitus, right greater than left. Right hip has decreased external and internal rotation but without pain. There is no joint heat, tenderness or erythema. 1. Describe in detail the pathophysiology of osteoarthritis. 2. What risk factors does this patient have that would predispose her to developing osteoarthritis? List two. 3. List two symptoms from the information presented this patient has that can be directly correlated with osteoarthritis. 4. What are two other symptoms not presented in this case study that are typically seen in patients with osteoarthritis? 5. What are two important questions to ask her about her lifestyle and social history? 6. What are one positive and one negative finding gained during the physical exam?
A 74 year old woman has an appointment at the clinic where you work. She is complaining of aching in her knees, the right being worse than the left and the pain is worse when it rains. She states the knee pain has been going on for several years. She now is having difficulty climbing the stairs in her home. In addition she has had low back pain for many years. She suffered a broken right hip 3 years ago when she fell on an icy sidewalk. Her knees started to become significantly more painful after she gained 15 pounds over the last 6 months. She played field hockey in college and had a right knee injury at that time, but it never needed surgery. Her joints are the most stiff after she has been sitting or lying still – the "loosen up" with activity. Her back pain doesn't seem to be getting any worse and her hip seems to have healed well. She denies any numbness, weakness or shooting pains in her legs. She takes ibuprofen 400 mg QID with some relief, but it gives her indigestion. She denies any cardiac, lung or renal diseases and has never had an ulcer or blood in her stool. She had a hysterectomy 25 years ago and does not take any hormones. She takes no prescribed medications and has no allergies. She exercises regularly in the pool but no longer walks daily as she had in the past. She has a well-balanced diet but it is high in prepared food and soft drinks and low in calcium. She does not smoke and drinks 1-2 alcohol drinks each evening. She lives in a 2 story home on the outskirts of town with her 68 year old sister. Upon musculoskeletal examination you discover she has full passive and active range of motion at the shoulders and elbows. There is decreased range of motion and Bouchard's and Heberden's nodes in bilateral hand exam. Her back has decreased flexion and extension with mild scoliosis. Both knees are enlarged with decreased range of motion and crepitus, right greater than left. Right hip has decreased external and internal rotation but without pain. There is no joint heat, tenderness or erythema. 1. Describe in detail the pathophysiology of osteoarthritis. 2. What risk factors does this patient have that would predispose her to developing osteoarthritis? List two. 3. List two symptoms from the information presented this patient has that can be directly correlated with osteoarthritis. 4. What are two other symptoms not presented in this case study that are typically seen in patients with osteoarthritis? 5. What are two important questions to ask her about her lifestyle and social history? 6. What are one positive and one negative finding gained during the physical exam?



