Transcribed Image Text from this Question
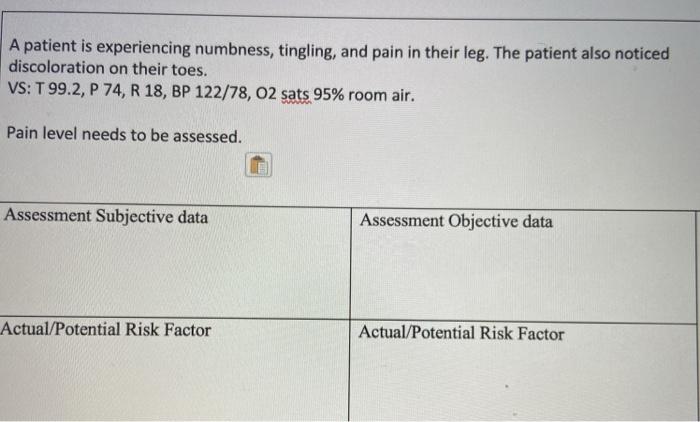
A patient is experiencing numbness, tingling, and pain in their leg. The patient also noticed discoloration on their toes. VS: T 99.2, P 74, R 18, BP 122/78, 02 sats 95% room air. Pain level needs to be assessed. Assessment Subjective data Assessment Objective data Actual/Potential Risk Factor Actual/Potential Risk Factor
(Visited 4 times, 1 visits today)
Related posts:
- Question: Patient Information General Survey Information: Patient Complains Of Breathlessness, Nocturia, & Fatigue For Past 2 Weeks. The Patient States That Their Ankles Look Like Melons After Working All Day And Has Been Experiencing Dizziness & Palpations X 2 Days. VS: T 98.6, P 130, R 22, BP 96/60, O2 Sats 91% Room Air Pain Level To Be Assessed. Assessment …
- Question: Soap Note Cardiacplease Write It In Full Sentencesthank YouS Is Subjective, Please Write 5 Subjective Questions You Can Ask Your Patient Specific To This Topic O Is Objective, Please List 5 Objective Assessments To Aid In Making A Clinical Judgement A Is Assessment Please List 5 Potential Red Flags That One Can Find During This Assessment P Is …
- Question: Soap Note AbdomenIn Full Sentence Please Thank You.S Is Subjective, Please Write 5 Subjective Questions You Can Ask Your Patient Specific To This TopicO Is Objective, Please List 5 Objective Assessments To Aid In Making A Clinical Judgement A Is Assessment Please List 5 Potential Red Flags That One Can Find During This AssessmentP Is Plan, Please List …
- Question: Saop Notes On CardiacS Is Subjective, Please Write 5 Subjective Questions You Can Ask Your Patient Specific To This TopicO Is Objective, Please List 5 Objective Assessments To Aid In Making A Clinical Judgement A Is Assessment Please List 5 Potential Red Flags That One Can Find During This AssessmentP Is Plan, Please List 5 Things You Can Educate Your …
- Question: Skills Lab Virtual Scenario- Head To Toe Assessment With Follow Up You Have Just Conducted A Head-to-toe Assessment On Your Patient. The Assessment Showed Abnormal Objective And Subjective Findings, Both Requiring Nursing Documentation & Actions. During The Assessment You Noted The Following: Objective Data: Patient Is AAOx1, Pleasant And Cooperative …
- Question: 7:20 Done Attachment Concerny After A Couple Moments Of Resting His O2 Sats Are Now 91%. You Back To His Room Where He Sits In The Chair Waiting For Lunch. You Reassess His Lungs And He Now Has Expiratory Wheezes Bilaterally Throughout Both Lung Fields. His O2 Sats Are Now 88%. You Decide That Respiratory Therapy Should Be Called To Administer An Albuterol …
- Question: The Mother Is17 Years Old The Mother’s Vital Signs: T = 97.8 F Oral BP = 122/68 P = 86 RR = 20 O2 Sat = 98% (room Air) Pain Level = 2/10; Uterine Cramping Heart Sounds: Regular Lung Sounds: Clear Breasts: Full; No Tenderness; No Masses Fundus: Mild Contractions Noted Every 5 Minutes Cervix Dilated 3 Cm; 50% Effaced Bowel Sounds: Active Bladder: Non-distended…
- Question: 2. Mr. Granger Is A 23yearoid Admitted To Your Unit With A C5-C6 Spinal Cord Injury After A Motor Vehicle Crash The Following Data Is Collected Subjective Pain In The Cervical Spine No Sensation Below The Level Of Injury Objective No Movement Below The Level Of Injury Blood Pressure 80/60 Pulse 45 Beats Per Minute Respirations Shallow Temperature 97 …
- Question: A 45-year-old Woman With A History Of Inhalant Abuse Presents To The Emergency Room Complaining Of Dyspnea. She Has An SpO2 Of 99% On Room Air And Is Obviously Tachypneic On Exam With What Appears To Be Kussmaul’s Respirations. A Room Air Arterial Blood Gas Is Performed And Reveals: PH 6.95, PCO2 19 MmHg, PO2 128 MmHg, HCO3 2 MEq/L A Chemistry Panel …
- Question: Case: Dizziness K.P. Is A 72-year-old Female Who Complains Of Dizziness. Subjective Data States She Has Had Dizziness For 2 Weeks, Worse In Morning Feels Like The Room Is Spinning Difficulty Walking Feels Lightheaded Usually Able To Drive, Not At Present Denies Blurry Vision, Nausea, Or Vomiting Objective Data Able To Reproduce Sensation By Moving Head …



