Transcribed Image Text from this Question
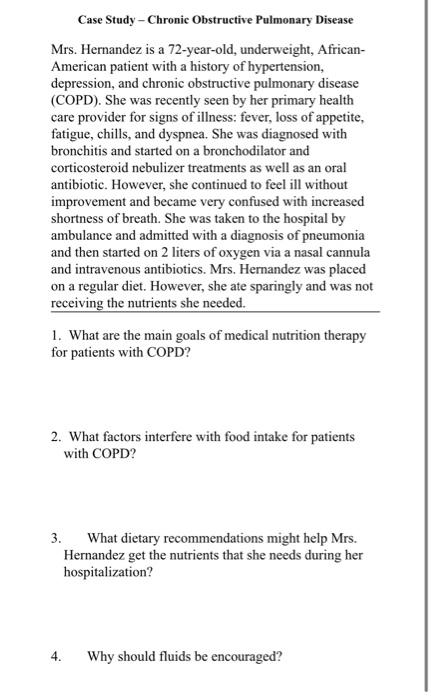
Case Study – Chronic Obstructive Pulmonary Disease Mrs. Hernandez is a 72-year-old, underweight, African- American patient with a history of hypertension, depression, and chronic obstructive pulmonary disease (COPD). She was recently seen by her primary health care provider for signs of illness: fever, loss of appetite, fatigue, chills, and dyspnea. She was diagnosed with bronchitis and started on a bronchodilator and corticosteroid nebulizer treatments as well as an oral antibiotic. However, she continued to feel ill without improvement and became very confused with increased shortness of breath. She was taken to the hospital by ambulance and admitted with a diagnosis of pneumonia and then started on 2 liters of oxygen via a nasal cannula and intravenous antibiotics. Mrs. Hernandez was placed on a regular diet. However, she ate sparingly and was not receiving the nutrients she needed. 1. What are the main goals of medical nutrition therapy for patients with COPD? 2. What factors interfere with food intake for patients with COPD? 3. What dietary recommendations might help Mrs. Hernandez get the nutrients that she needs during her hospitalization? 4. Why should fluids be encouraged?
(Visited 6 times, 1 visits today)



