Transcribed Image Text from this Question
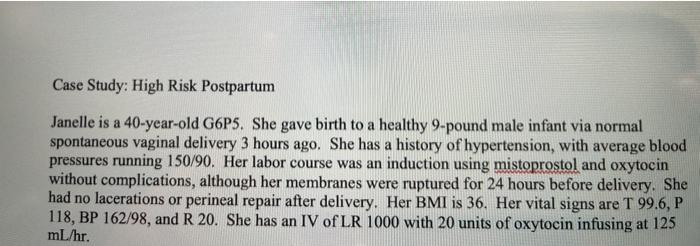
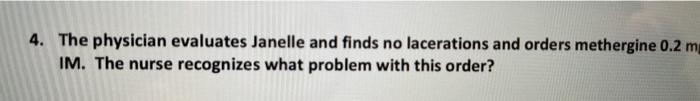
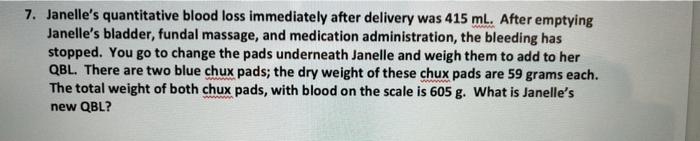
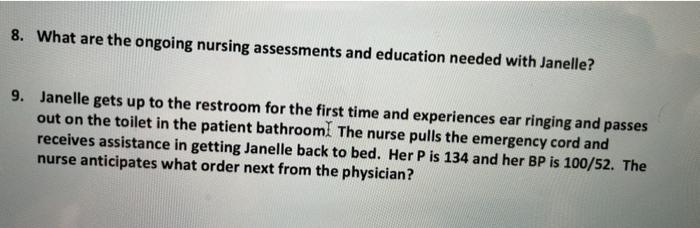
Case Study: High Risk Postpartum Janelle is a 40-year-old G6P5. She gave birth to a healthy 9-pound male infant via normal spontaneous vaginal delivery 3 hours ago. She has a history of hypertension, with average blood pressures running 150/90. Her labor course was an induction using mistoprostol and oxytocin without complications, although her membranes were ruptured for 24 hours before delivery. She had no lacerations or perineal repair after delivery. Her BMI is 36. Her vital signs are T 99.6, P 118, BP 162/98, and R 20. She has an IV of LR 1000 with 20 units of oxytocin infusing at 125 mL/hr. 4. The physician evaluates Janelle and finds no lacerations and orders methergine 0.2 m IM. The nurse recognizes what problem with this order? 7. Janelle’s quantitative blood loss immediately after delivery was 415 ml. After emptying Janelle’s bladder, fundal massage, and medication administration, the bleeding has stopped. You go to change the pads underneath Janelle and weigh them to add to her QBL. There are two blue chux pads; the dry weight of these chux pads are 59 grams each. The total weight of both chux pads, with blood on the scale is 605 g. What is Janelle’s new QBL? 8. What are the ongoing nursing assessments and education needed with Janelle? 9. Janelle gets up to the restroom for the first time and experiences ear ringing and passes out on the toilet in the patient bathroomI The nurse pulls the emergency cord and receives assistance in getting Janelle back to bed. Her P is 134 and her BP is 100/52. The nurse anticipates what order next from the physician?
(Visited 3 times, 1 visits today)



