Transcribed Image Text from this Question
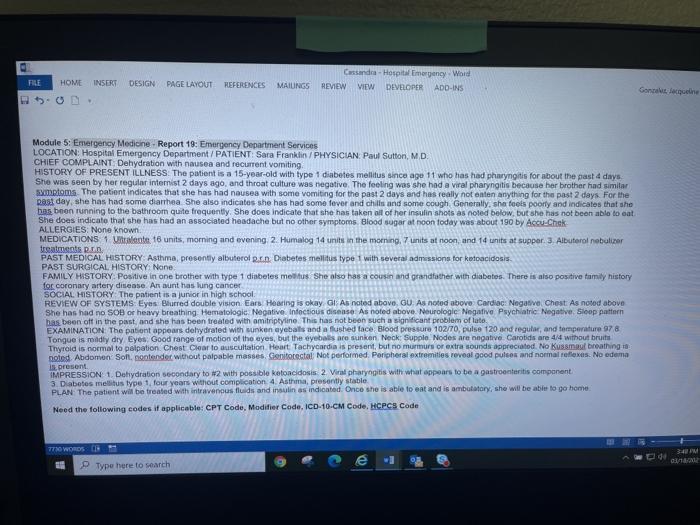
FILE HOME INSERT DESIGN PAGE LAYOUT Cassandra – Hospital Emergency Word REVIEW VIEW DEVELOPER ADD-INS REFERENCES MAIUNGS Gonne Module 5: Emergency Medicine – Report 19: Emergency Department Services LOCATION: Hospital Emergency Department / PATIENT: Sara Franklin / PHYSICIAN. Paul Sutton, MD CHIEF COMPLAINT Dehydration with nausea and recurrent vomiting HISTORY OF PRESENT ILLNESS. The patient is a 15-year-old with type 1 diabetes mellitus since age 11 who has had pharyngitis for about the past 4 days She was seen by her regular intemist 2 days ago, and throat culture was negative. The feeling was she had a viral pharyngitis because her brother had similar symptoms. The patient indicates that she has had nausea with some vomiting for the past 2 days and has really not enten anything for the past 2 days. For the Rasi day, she has had some diarrhea. She also indicates she has had some fever and chills and some cough Generally, she fools poorly and indicates that she has been running to the bathroom quite frequently. She does indicate that she has taken all of her insulin shots as noted below, but she has not been able to eat She does indicate that she has had an associated headache but no other symptoms. Blood sugar at noon today was about 190 by Accu-Chek ALLERGIES: None known MEDICATIONS 1 Utente 16 units, morning and evening 2. Humalog 14 units in the morning. 7 units at noon, and 14 units at supper. 3. Albuterol nebulizer treatments DID PAST MEDICAL HISTORY Asthma, presently albuterol Dan Diabetes mellitus type 1 with several admissions for ketoacidosis. PAST SURGICAL HISTORY None FAMILY HISTORYPositive in one brother with type 1 diabetes mellitus. She also has a cousin and grandfather with diabetes. There is also positive family history for coronary artery disease. An aunt has lung cancer SOCIAL HISTORY The patient is a junior in high school REVIEW OF SYSTEMS Eyes Blurred double vision Ears Hearing is okay Gl: As noted above. GU. As noted above Cardiac: Negative Chest As noted above She has had no SOB or heavy breathing Hematologic Negative Infectious disease As noted above. Neurologic Negative Psychiatric Negative. Sloop pattern has been off in the past, and she has been treated with amitriptyline. This has not been such a significant problem of late. EXAMINATION The patient appears dehydrated with sunken eyeballs and a flushed face Blood pressure 102/70, pulse 120 and regular and temperature 978 Tongue is madly dry Eyes Good range of motion of the eyes, but the eyeballs are sunker Neck Supple. Nodes are negative Carotid are 4 without brut Thyroid is normal to palpation Chest Clear to auscultation Heart Tachycardia is present, but no murmurs or extra sounds appreciated. No Kussmauf breathing is noted. Abdomon Solt, nootendet without palpable masses. Contorectal Not performed. Poripheral extremities reveal good pulses and normal refoxes. No edema is present IMPRESSION 1. Dohydration secondary to #2 with possible ketoacidosis 2 Vinapharyngitis with what appears to be a gastroenteritis component 3. Diabetes mellitus type 1, four years without complication 4. Asthma, presently stable PLAN The patient will be treated with intravenous fluids and insulin as indicated. Once she is able to eat and is ambulatory, she will be able to go home Need the following codes if applicable: CPT Code, Modifier Code, ICD-10-CM Code, HCPCS Code 7TH WORDS 343 PM Pd Type here to search
(Visited 4 times, 1 visits today)



