Transcribed Image Text from this Question
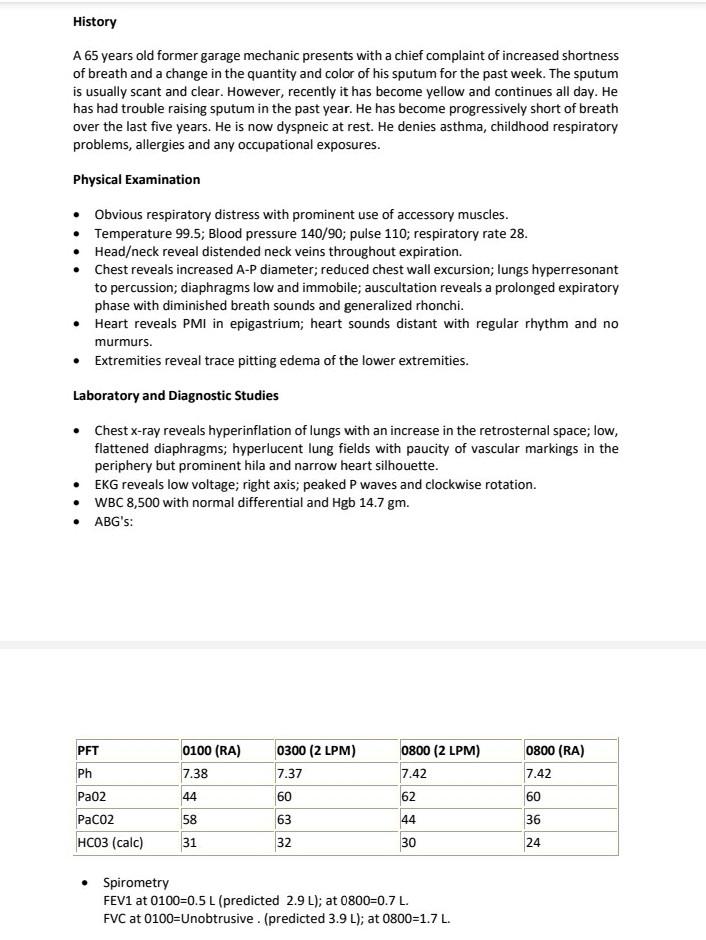
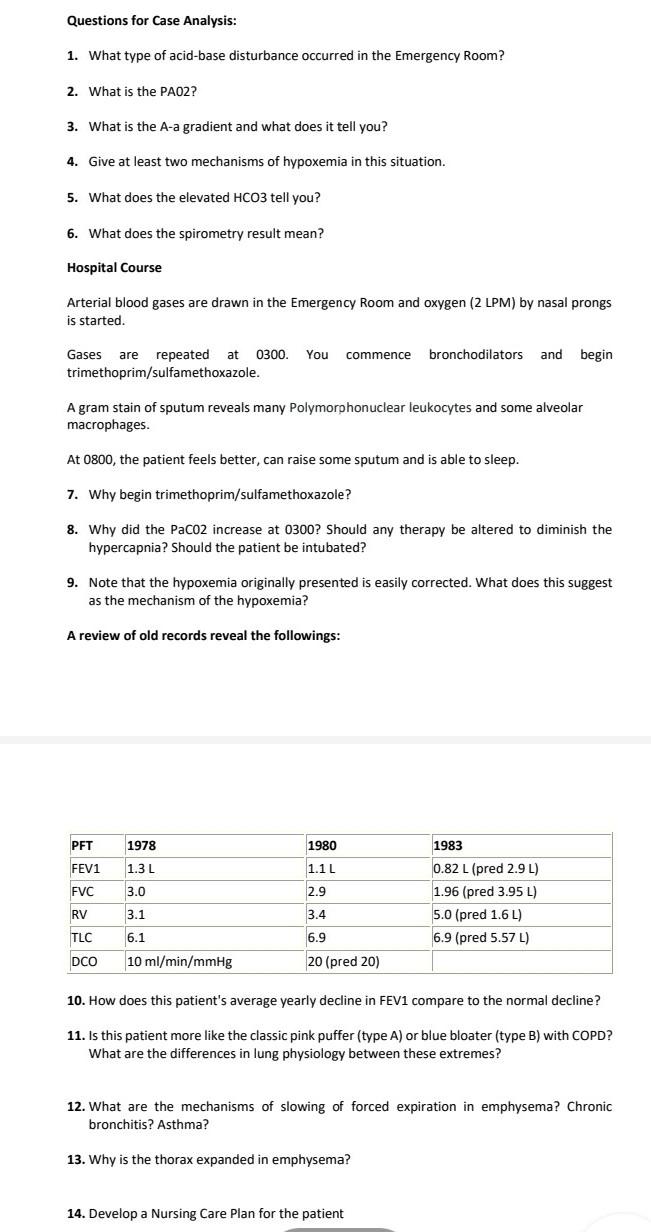
History A 65 years old former garage mechanic presents with a chief complaint of increased shortness of breath and a change in the quantity and color of his sputum for the past week. The sputum is usually scant and clear. However, recently it has become yellow and continues all day. He has had trouble raising sputum in the past year. He has become progressively short of breath over the last five years. He is now dyspneic at rest. He denies asthma, childhood respiratory problems, allergies and any occupational exposures. Physical Examination Obvious respiratory distress with prominent use of accessory muscles. Temperature 99.5; Blood pressure 140/90; pulse 110; respiratory rate 28. Head/neck reveal distended neck veins throughout expiration. Chest reveals increased A-P diameter; reduced chest wall excursion; lungs hyperresonant to percussion; diaphragms low and immobile; auscultation reveals a prolonged expiratory phase with diminished breath sounds and generalized rhonchi. Heart reveals PMI in epigastrium; heart sounds distant with regular rhythm and no murmurs. • Extremities reveal trace pitting edema of the lower extremities. Laboratory and Diagnostic Studies Chest x-ray reveals hyperinflation of lungs with an increase in the retrosternal space; low, flattened diaphragms; hyperlucent lung fields with paucity of vascular markings in the periphery but prominent hila and narrow heart silhouette. EKG reveals low voltage; right axis; peaked P waves and clockwise rotation. WBC 8,500 with normal differential and Hgb 14.7 gm. ABG’s: 0300 (2 LPM) 0800 (RA) PFT Ph 0100 (RA) 7.38 0800 (2 LPM) 7.42 7.37 7.42 Pa02 44 60 62 60 PaCo2 58 63 44 36 HCO3 (calc) 31 32 30 24 Spirometry FEV1 at 0100=0.5 L (predicted 2.9 L); at 0800=0.7 L. FVC at 0100=Unobtrusive. (predicted 3.9 L); at 0800=1.7 L. Questions for Case Analysis: 1. What type of acid-base disturbance occurred in the Emergency Room? 2. What is the PAO2? 3. What is the A-a gradient and what does it tell you? 4. Give at least two mechanisms of hypoxemia in this situation. 5. What does the elevated HCO3 tell you? 6. What does the spirometry result mean? Hospital Course Arterial blood gases are drawn in the Emergency Room and oxygen (2 LPM) by nasal prongs is started. commence bronchodilators and begin Gases are repeated at 0300. You trimethoprim/sulfamethoxazole. A gram stain of sputum reveals many Polymorphonuclear leukocytes and some alveolar macrophages. At 0800, the patient feels better, can raise some sputum and is able to sleep. 7. Why begin trimethoprim/sulfamethoxazole? 8. Why did the Paco2 increase at 0300? Should any therapy be altered to diminish the hypercapnia? Should the patient be intubated? 9. Note that the hypoxemia originally presented is easily corrected. What does this suggest as the mechanism of the hypoxemia? A review of old records reveal the followings: 1978 1980 1983 PFT FEV1 FVC 1.3 L 1.1 L 2.9 3.0 3.1 0.82 L (pred 2.9 L) 1.96 (pred 3.95 L) 5.0 (pred 1.6L) 6.9 (pred 5.57L) RV 3.4 TLC 6.1 6.9 20 (pred 20) DCO 10 ml/min/mmHg 10. How does this patient’s average yearly decline in FEV1 compare to the normal decline? 11. Is this patient more like the classic pink puffer (type A) or blue bloater (type B) with COPD? What are the differences in lung physiology between these extremes? 12. What are the mechanisms of slowing of forced expiration in emphysema? Chronic bronchitis? Asthma? 13. Why is the thorax expanded in emphysema? 14. Develop a Nursing Care Plan for the patient
(Visited 11 times, 1 visits today)