Transcribed Image Text from this Question
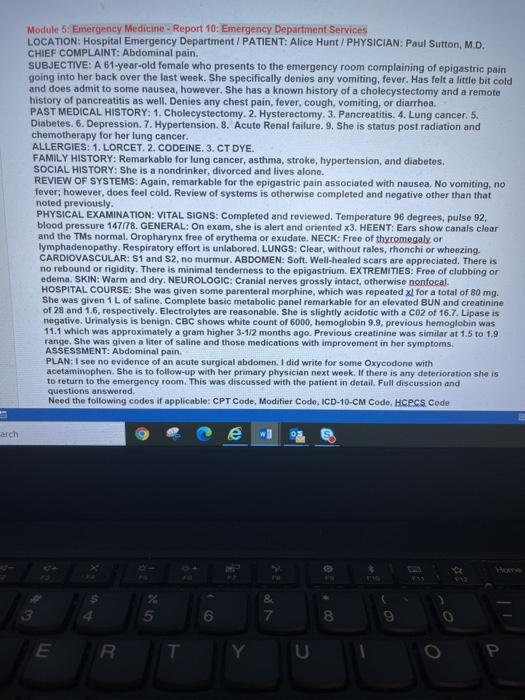
Module 5: Emergency Medicine – Report 10: Emergency Department Services LOCATION: Hospital Emergency Department / PATIENT: Alice Hunt / PHYSICIAN: Paul Sutton, M.D. CHIEF COMPLAINT: Abdominal pain. SUBJECTIVE: A 61-year-old female who presents to the emergency room complaining of epigastric pain going into her back over the last week. She specifically denies any vomiting, fever. Has felt a little bit cold and does admit to some nausea, however. She has a known history of a cholecystectomy and a remote history of pancreatitis as well. Denies any chest pain, fever, cough, vomiting, or diarrhea. PAST MEDICAL HISTORY: 1. Cholecystectomy. 2. Hysterectomy. 3. Pancreatitis. 4. Lung cancer. 5. Diabetes. 6. Depression. 7. Hypertension. 8. Acute Renal failure. 9. She is status post radiation and chemotherapy for her lung cancer. ALLERGIES: 1. LORCET. 2. CODEINE. 3. CT DYE. FAMILY HISTORY: Remarkable for lung cancer, asthma, stroke, hypertension, and diabetes. SOCIAL HISTORY: She is a nondrinker, divorced and lives alone. REVIEW OF SYSTEMS: Again, remarkable for the epigastric pain associated with nausea. No vomiting, no fever, however, does feel cold. Review of systems is otherwise completed and negative other than that noted previously. PHYSICAL EXAMINATION: VITAL SIGNS: Completed and reviewed. Temperature 96 degrees, pulse 92, blood pressure 147178. GENERAL: On exam, she is alert and oriented X3. HEENT: Ears show canals clear and the TMs normal. Oropharynx free of erythema or exudate. NECK: Free of thyromegaly, or lymphadenopathy. Respiratory effort is unlabored. LUNGS: Clear, without rales, rhonchi or wheezing. CARDIOVASCULAR: S1 and 52, no murmur. ABDOMEN: Soft. Well-healed scars are appreciated. There is no rebound or rigidity. There is minimal tenderness to the epigastrium. EXTREMITIES: Free of clubbing or edema. SKIN: Warm and dry. NEUROLOGIC: Cranial nerves grossly intact, otherwise nonfocal HOSPITAL COURSE: She was given some parenteral morphine, which was repeated xl for a total of 80 mg. She was given 1 L of saline. Complete basic metabolic panel remarkable for an elevated BUN and creatinine of 28 and 1.6, respectively. Electrolytes are reasonable. She is slightly acidotic with a CO2 of 16.7. Lipase is negative. Urinalysis is benign. CBC shows white count of 6000, hemoglobin 9.9. previous hemoglobin was 11.1 which was approximately a gram higher 3-1/2 months ago. Previous creatinine was similar at 1.5 to 1.9 range. She was given a liter of saline and those medications with improvement in her symptoms ASSESSMENT: Abdominal pain. PLAN: I see no evidence of an acute surgical abdomen. I did write for some Oxycodone with acetaminophen. She is to follow-up with her primary physician next week. If there is any deterioration she is to return to the emergency room. This was discussed with the patient in detail. Full discussion and questions answered. Need the following codes if applicable: CPT Code, Modifier Code, ICD-10-CM Code, HCPCS Code arch e 8 7 5 6 8 9 E R U
(Visited 3 times, 1 visits today)



