Mr. Li is receiving skilled physical therapy. He is doing well.The therapist is in the facility. She is running behind schedule incompleting an assessment on a new resident. She asks you to performrange of motion exercises on Mr. Li. The resident had hip surgerytwo weeks ago. What will you do? On the other hand make a anotherparagraph and discuss the Mr. Martinez is on a bedmobility program. He has a trapeze at the head of the bed. Explainhow you will teach him to move to the head and foot of the bedusing the trapeze. Where does the restorative nursing assistantfind information about the resident’s range of motion? own simplewords
Transcribed Image Text from this Question
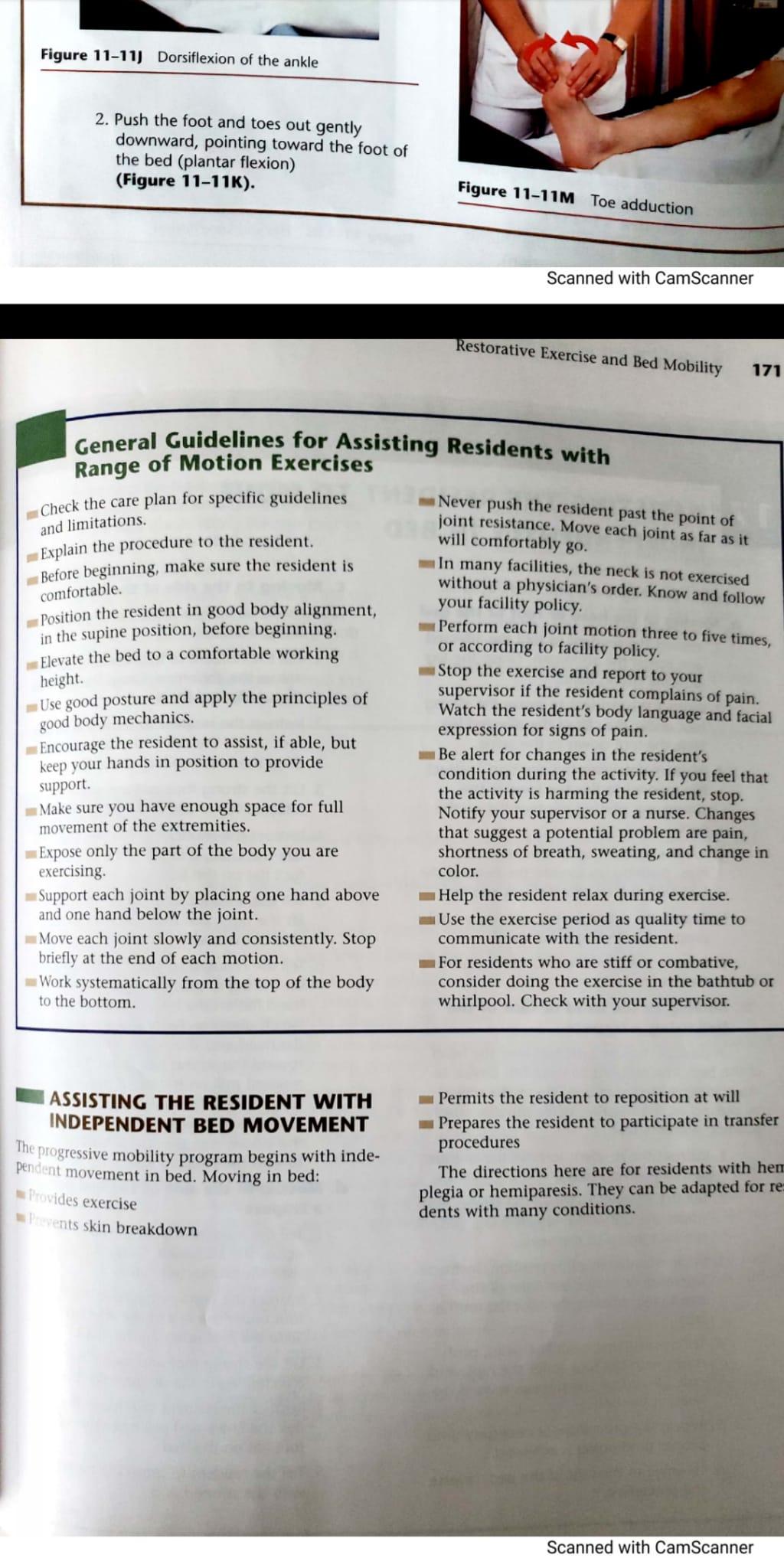
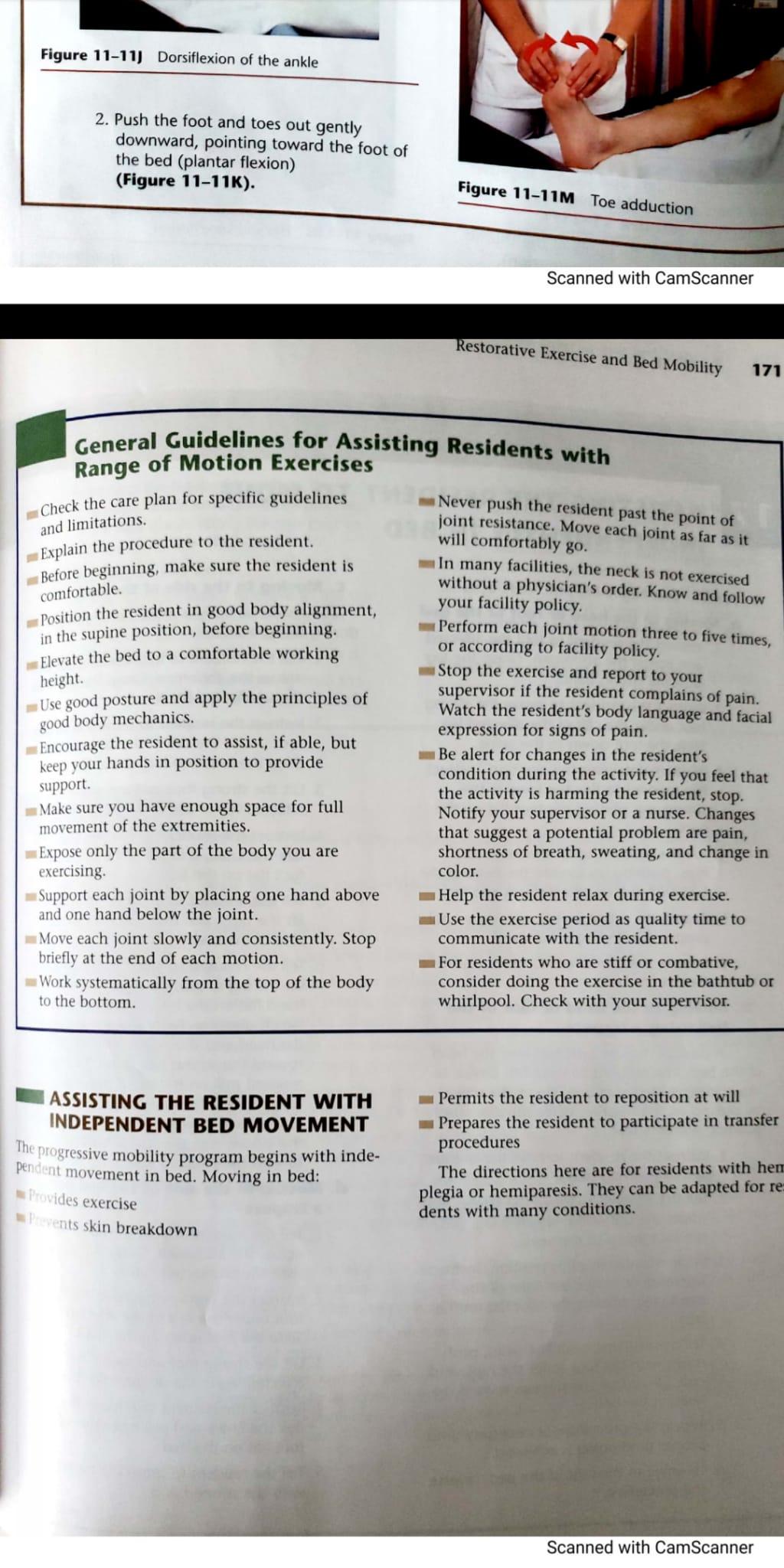
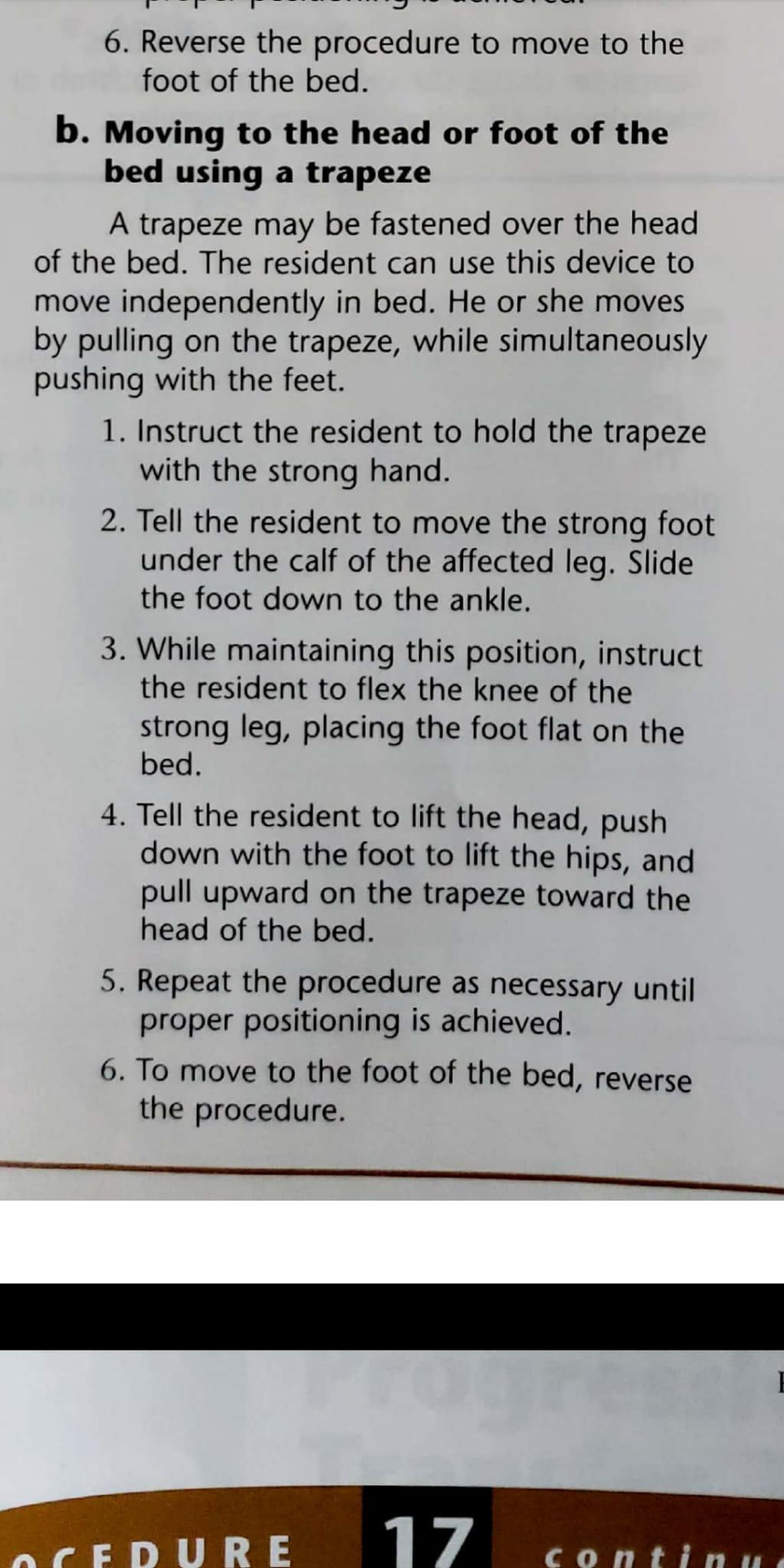
5. Repeat the procedure as necessary until proper positioning is achieved. 6. To move to the foot of the bed, reverse the procedure. flex the knee, and place the sole of the foot flat on the bed. 5. Tell the resident to grasp the trapeze with the strong hand. Scanned with CamScanner Restorative Exercise and Bed Mobility 173 17 OCEDURE continued 6. Instruct the resident to pull on the trapeze, while simultaneously pushing the foot down, lifting the hips over to the desired side of the bed. e. Turning to the sides 1. Instruct the resident to move to the side of the bed opposite the direction in which he or she wishes to turn, following the directions in step cor d. 2. If the resident will be turning onto the affected side, have him or her grab the leg on that side with the strong hand and pull his or her body over. If the resident will be turning onto the strong side, instruct him or her to grasp the affected hand with the strong hand. Extend the arm and lock the elbow. Raise the arms in the air. Using the strong arm, swing the body over onto the strong side. 2. Perform your procedure completion actions. Y POINTS CHAPTER Residents in the long-term care facility need exercise for their overall health and well-being. Begin the exercise program gradually, increasing as the resident develops endurance. Monitor the pulse during exercise, stopping if the rate exceeds 100. Exercising a joint several times a day is better than exercising it once. Therapeutic exercises are specifically planned for individual residents to maintain or improve joint function. The purpose of therapeutic exercises is to prevent and correct deformities, diseases, and injuries. Range of motion is the normal movement of the joints. It is affected by age, body size, genetics, activity, and the presence or absence of disease. Range of motion exercises prevent contractures and deformities, improve circulation, and enhance the resident’s sense of well-being. Active range of motion exercises are done by residents each day during movement, ADLs, certain activities, and in exercise groups. Active assisted range of motion exercises are done when the resident needs assistance moving because of paralysis, paresis, weakness, pain, serious heart problems, or increased spasticity. The exercises are either started or completed by the resident. Passive range of motion exercises are performed for residents with conditions such as paralysis, contractures, orthopedic and neurologic disorders, and severe cognitive impairment, or when independent movement is impossible. Resistive range of motion exercises are prescribed by the licensed therapist to increase strength. The progressive mobility program begins with teaching residents how to move independently in bed, providing exercise, preventing skin breakdown, and preparing the resident to participate in transfer procedures. Scanned with CamScanner Figure 11-111 Dorsiflexion of the ankle 2. Push the foot and toes out gently downward, pointing toward the foot of the bed (plantar flexion) (Figure 11-11K). Figure 11-11M Toe adduction Scanned with CamScanner Restorative Exercise and Bed Mobility 171 General Guidelines for Assisting Residents with Range of Motion Exercises Check the care plan for specific guidelines Never push the resident past the point of joint resistance. Move each joint as far as it and limitations, Explain the procedure to the resident will comfortably go. Before beginning, make sure the resident is In many facilities, the neck is not exercised without a physician’s order. Know and follow comfortable. Position the resident in good body alignment, your facility policy Perform each joint motion three to five times, in the supine position, before beginning. Elevate the bed to a comfortable working or according to facility policy. Stop the exercise and report to your height. Use good posture and apply the principles of supervisor if the resident complains of pain. Watch the resident’s body language and facial good body mechanics. expression for signs of pain. Encourage the resident to assist, if able, but keep your hands in position to provide Be alert for changes in the resident’s condition during the activity. If you feel that support. the activity is harming the resident, stop. Make sure you have enough space for full Notify your supervisor or a nurse. Changes movement of the extremities. that suggest a potential problem are pain, Expose only the part of the body you are shortness of breath, sweating, and change in exercising. color. Support each joint by placing one hand above Help the resident relax during exercise. and one hand below the joint. Use the exercise period as quality time to Move each joint slowly and consistently. Stop communicate with the resident. briefly at the end of each motion. For residents who are stiff or combative, Work systematically from the top of the body consider doing the exercise in the bathtub or to the bottom whirlpool. Check with your supervisor. ASSISTING THE RESIDENT WITH INDEPENDENT BED MOVEMENT The progressive mobility program begins with inde- pendent movement in bed. Moving in bed: – Permits the resident to reposition at will Prepares the resident to participate in transfer procedures The directions here are for residents with hem plegia or hemiparesis. They can be adapted for re- dents with many conditions. Provides exercise Prevents skin breakdown Scanned with CamScanner Figure 11-111 Dorsiflexion of the ankle 2. Push the foot and toes out gently downward, pointing toward the foot of the bed (plantar flexion) (Figure 11-11K). Figure 11-11M Toe adduction Scanned with CamScanner Restorative Exercise and Bed Mobility 171 General Guidelines for Assisting Residents with Range of Motion Exercises Check the care plan for specific guidelines Never push the resident past the point of joint resistance. Move each joint as far as it and limitations, Explain the procedure to the resident will comfortably go. Before beginning, make sure the resident is In many facilities, the neck is not exercised without a physician’s order. Know and follow comfortable. Position the resident in good body alignment, your facility policy Perform each joint motion three to five times, in the supine position, before beginning. Elevate the bed to a comfortable working or according to facility policy. Stop the exercise and report to your height. Use good posture and apply the principles of supervisor if the resident complains of pain. Watch the resident’s body language and facial good body mechanics. expression for signs of pain. Encourage the resident to assist, if able, but keep your hands in position to provide Be alert for changes in the resident’s condition during the activity. If you feel that support. the activity is harming the resident, stop. Make sure you have enough space for full Notify your supervisor or a nurse. Changes movement of the extremities. that suggest a potential problem are pain, Expose only the part of the body you are shortness of breath, sweating, and change in exercising. color. Support each joint by placing one hand above Help the resident relax during exercise. and one hand below the joint. Use the exercise period as quality time to Move each joint slowly and consistently. Stop communicate with the resident. briefly at the end of each motion. For residents who are stiff or combative, Work systematically from the top of the body consider doing the exercise in the bathtub or to the bottom whirlpool. Check with your supervisor. ASSISTING THE RESIDENT WITH INDEPENDENT BED MOVEMENT The progressive mobility program begins with inde- pendent movement in bed. Moving in bed: – Permits the resident to reposition at will Prepares the resident to participate in transfer procedures The directions here are for residents with hem plegia or hemiparesis. They can be adapted for re- dents with many conditions. Provides exercise Prevents skin breakdown Scanned with CamScanner 6. Reverse the procedure to move to the foot of the bed. b. Moving to the head or foot of the bed using a trapeze A trapeze may be fastened over the head of the bed. The resident can use this device to move independently in bed. He or she moves by pulling on the trapeze, while simultaneously pushing with the feet. 1. Instruct the resident to hold the trapeze with the strong hand. 2. Tell the resident to move the strong foot under the calf of the affected leg. Slide the foot down to the ankle. 3. While maintaining this position, instruct the resident to flex the knee of the strong leg, placing the foot flat on the bed. 4. Tell the resident to lift the head, push down with the foot to lift the hips, and pull upward on the trapeze toward the head of the bed. 5. Repeat the procedure as necessary until proper positioning is achieved. 6. To move to the foot of the bed, reverse the procedure. OCEDURE 17 continu
(Visited 2 times, 1 visits today)