be concise please
Transcribed Image Text from this Question
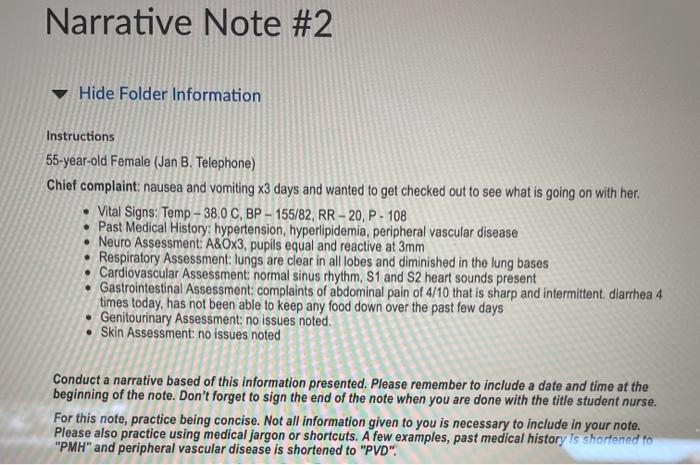
Narrative Note #2 Hide Folder Information Instructions 55-year-old Female (Jan B. Telephone) Chief complaint: nausea and vomiting x3 days and wanted to get checked out to see what is going on with her. • Vital Signs: Temp – 38.0 C, BP – 155/82, RR – 20, P. 108 • Past Medical History: hypertension, hyperlipidemia, peripheral vascular disease • Neuro Assessment: A&Ox3, pupils equal and reactive at 3mm • Respiratory Assessment: lungs are clear in all lobes and diminished in the lung bases • Cardiovascular Assessment: normal sinus rhythm, S1 and S2 heart sounds present • Gastrointestinal Assessment: complaints of abdominal pain of 4/10 that is sharp and intermittent diarrhea 4 times today, has not been able to keep any food down over the past few days • Genitourinary Assessment: no issues noted. • Skin Assessment: no issues noted Conduct a narrative based of this information presented. Please remember to include a date and time at the beginning of the note. Don’t forget to sign the end of the note when you are done with the title student nurse. For this note, practice being concise. Not all information given to you is necessary to include in your note. Please also practice using medical jargon or shortcuts. A few examples, past medical history is shortened to “PMH” and peripheral vascular disease is shortened to “PVD”
(Visited 3 times, 1 visits today)



