Transcribed Image Text from this Question
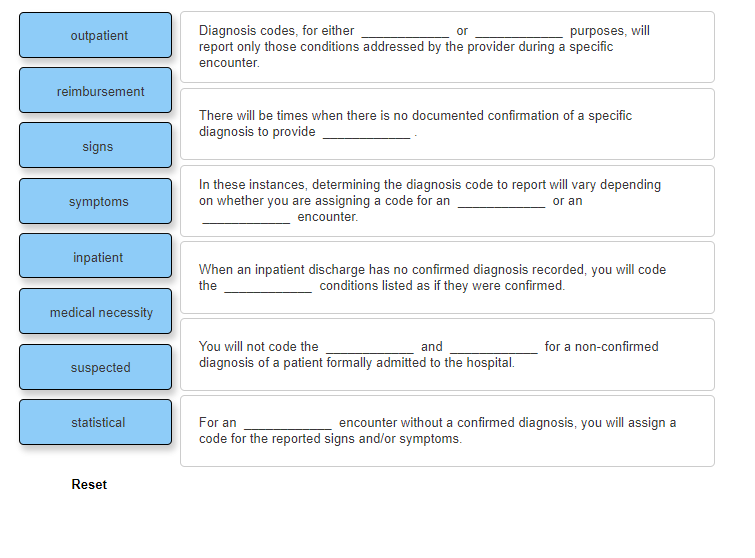
or outpatient Diagnosis codes, for either purposes, will report only those conditions addressed by the provider during a specific encounter. reimbursement There will be times when there is no documented confirmation of a specific diagnosis to provide signs symptoms In these instances, determining the diagnosis code to report will vary depending on whether you are assigning a code for an encounter. or an inpatient When an inpatient discharge has no confirmed diagnosis recorded, you will code the conditions listed as if they were confirmed. medical necessity for a non-confirmed You will not code the and diagnosis of a patient formally admitted to the hospital. suspected statistical For an encounter without a confirmed diagnosis, you will assign a code for the reported signs and/or symptoms. Reset
(Visited 2 times, 1 visits today)