Transcribed Image Text from this Question
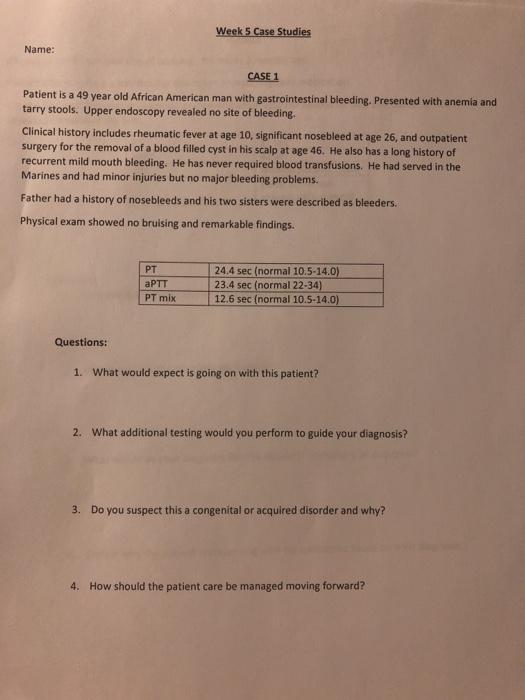
Week 5 Case Studies Name: CASE 1 Patient is a 49 year old African American man with gastrointestinal bleeding. Presented with anemia and tarry stools. Upper endoscopy revealed no site of bleeding. Clinical history includes rheumatic fever at age 10, significant nosebleed at age 26, and outpatient surgery for the removal of a blood filled cyst in his scalp at age 46. He also has a long history of recurrent mild mouth bleeding. He has never required blood transfusions. He had served in the Marines and had minor injuries but no major bleeding problems. Father had a history of nosebleeds and his two sisters were described as bleeders. Physical exam showed no bruising and remarkable findings. PT aPTT PT mix 24.4 sec (normal 10.5-14.0) 23.4 sec (normal 22-34) 12.6 sec (normal 10.5-14.0) Questions: 1. What would expect is going on with this patient? 2. What additional testing would you perform to guide your diagnosis? 3. Do you suspect this a congenital or acquired disorder and why? 4. How should the patient care be managed moving forward?
(Visited 2 times, 1 visits today)



