Please help me with this discharge teaching plan for this client.please answer throughly.
Transcribed Image Text from this Question
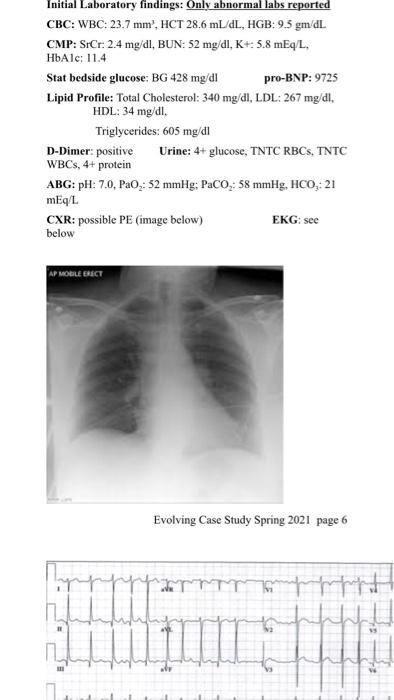
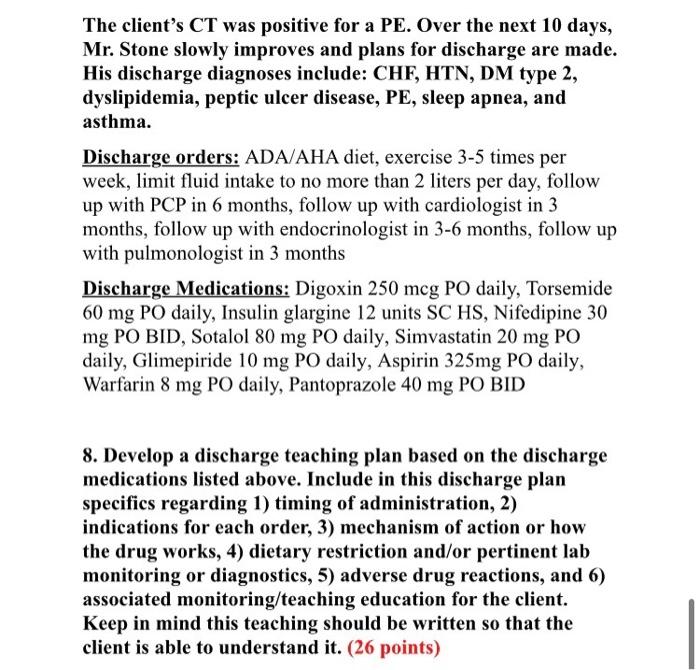
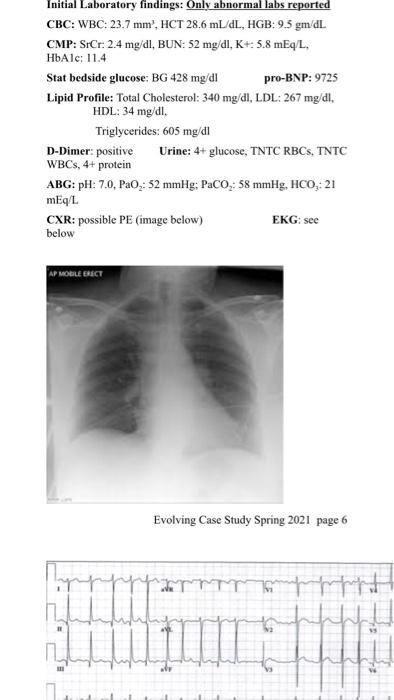
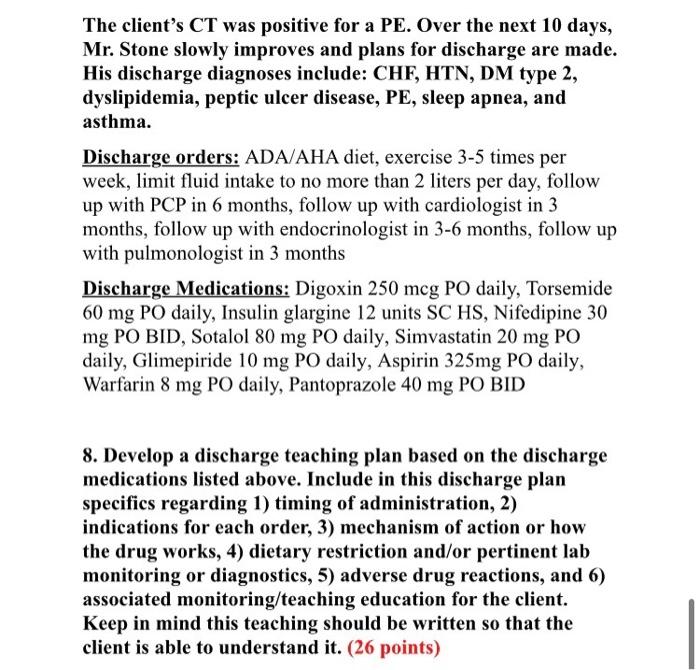
William Stone is a 71-year-old African-American male who presents to the emergency department with severe shortness of breath, which has progressively worsened over the previous week. Mr. Stone states that he had experienced chest discomfort rated a 4 out 0-10 pain scale last week. He also states “My legs are as big as tree trunks.” Past medical history includes: hypertension, Diabetes Mellitus Type 2 with the onset at age 43, sleep apnea, peptic ulcer disease, asthma, and obesity. Lipid profile unknown. Social History: smoking – 1 pk /day for 45 years, wife died 8 months ago, father of three children that all live out of state, retired 5 years ago from CFO position for a multinational company, and lives alone. Current meds: glipizide 5 mg daily, Glucophage 500 mg BID, amlodipine 10 mg daily, torsemide 40 mg daily, enteric-coated aspirin 325 mg daily, K-Dur 40 mEq daily, and pantoprazole 40 mg BID. Insurance: Medicare, no coinsurance. Mr. Stone states that it has been over a year since he saw his primary care provider and he has run out of most of his medications without the new prescriptions. Allergies: Ancef, Strawberries, & hydrocodone; all of which give him a rash. Religion: Catholic Upon admission to the ER, the following vital signs are obtained: Weight: 203 lbs., reported Height 5 ft. 10 in; computed BMI 29.1; T. 100.9°F: B/P 172/100; P 112 and irregular; RR 28; Pulse Ox on room air 90%. Admission assessment reveals: Well-developed, overweight male in moderate distress, skin dry and hot, PERRL, CN II-XII intact; Neurological exam: no deficits noted: Cardiac: S2 and Si clearly audible, with S3 audible with client lying on left side, Grade 4 diastolic murmur audible at apex, irregular rhythm, peripheral pulses palpable 2+; Pulmonary: Slight wheezing heard throughout A&P, with coarse crackles in bases bilaterally; Abdomen: obese, no tenderness noted, bowel sounds audible x 4; G/U: deferred; Extremities: 4+ pitting edema lower extremities, upper extremities 2+ edema. Skin: Braden scale: 15, yellowish bruising noted on left forearm Emergency department orders: Cardiac Enzymes x 3, Complete Blood Count with differential, Complete Metabolic Profile, HbAlc, Lipid Profile, 12-lead ECG, Stat BG, D-Dimer, pro-BNP, Chest x-ray, Urinalysis, ABGs Initial Laboratory findings: Only abnormal labs reported CBC: WBC: 23.7 mm’, HCT 28.6 mL/dL, HGB: 9.5 gm/dL CMP: SrCr: 2.4 mg/dl, BUN: 52 mg/dl, K+: 5.8 mEq/L, HbAlc: 11.4 Initial Laboratory findings: Only abnormal labs reported CBC: WBC: 23.7 mm’, HCT 28.6 mL/dL, HGB: 95 gm dL CMP: SrCr. 2.4 mg/dl, BUN: 52 mg/dl, K+: 5.8 mEq/L, HbAlc: 11.4 Stat bedside glucose: BG 428 mg/d! pro-BNP: 9725 Lipid Profile: Total Cholesterol: 340 mg/dl, LDL: 267 mg/dl. HDL: 34 mg/dl. Triglycerides: 605 mg/dl D-Dimer: positive Urine: 4+ glucose, TNTC RBCS, TNTC WBCs, 4+ protein ABG: pH: 7.0, PaO2: 52 mmHg; PaCO2: 58 mmHg, HCO, 21 mEq/L. CXR: possible PE (image below) EKG: see below AP MOBILE ERACY Evolving Case Study Spring 2021 page 6 The client’s CT was positive for a PE. Over the next 10 days, Mr. Stone slowly improves and plans for discharge are made. His discharge diagnoses include: CHF, HTN, DM type 2, dyslipidemia, peptic ulcer disease, PE, sleep apnea, and asthma. Discharge orders: ADA/AHA diet, exercise 3-5 times per week, limit fluid intake to no more than 2 liters per day, follow up with PCP in 6 months, follow up with cardiologist in 3 months, follow up with endocrinologist in 3-6 months, follow up with pulmonologist in 3 months Discharge Medications: Digoxin 250 mcg PO daily, Torsemide 60 mg PO daily, Insulin glargine 12 units SC HS, Nifedipine 30 mg PO BID, Sotalol 80 mg PO daily, Simvastatin 20 mg PO daily, Glimepiride 10 mg PO daily, Aspirin 325mg PO daily, Warfarin 8 mg PO daily, Pantoprazole 40 mg PO BID 8. Develop a discharge teaching plan based on the discharge medications listed above. Include in this discharge plan specifics regarding 1) timing of administration, 2) indications for each order, 3) mechanism of action or how the drug works, 4) dietary restriction and/or pertinent lab monitoring or diagnostics, 5) adverse drug reactions, and 6) associated monitoring/teaching education for the client. Keep in mind this teaching should be written so that the client is able to understand it. (26 points)
(Visited 2 times, 1 visits today)



