Transcribed Image Text from this Question
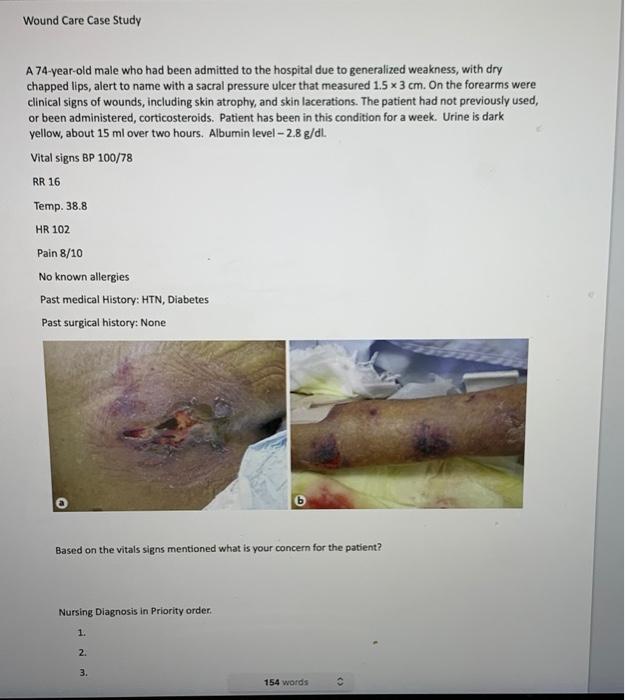
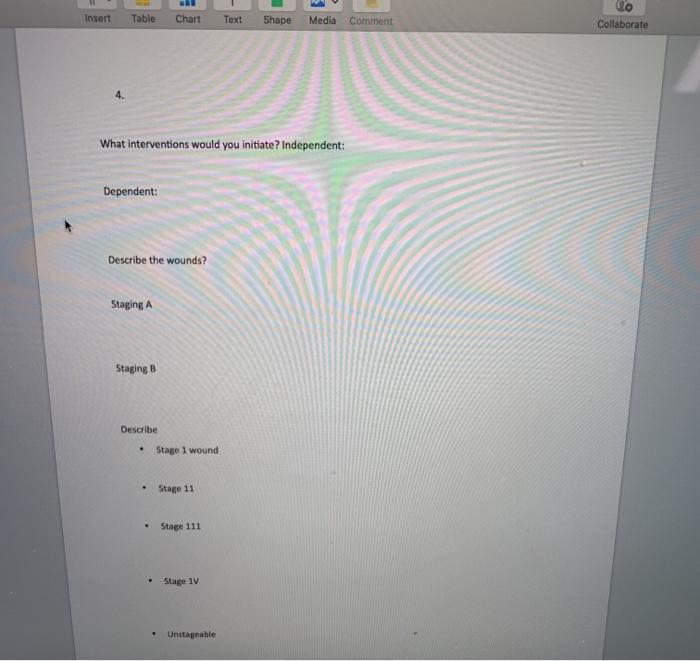
Wound Care Case Study A 74-year-old male who had been admitted to the hospital due to generalized weakness, with dry chapped lips, alert to name with a sacral pressure ulcer that measured 1.5 x 3 cm. On the forearms were clinical signs of wounds, including skin atrophy, and skin lacerations. The patient had not previously used, or been administered, corticosteroids. Patient has been in this condition for a week. Urine is dark yellow, about 15 ml over two hours. Albumin level – 2.8 g/dL Vital signs BP 100/78 RR 16 Temp. 38.8 HR 102 Pain 8/10 No known allergies Past medical History: HTN, Diabetes Past surgical history: None Based on the vitals signs mentioned what is your concern for the patient? Nursing Diagnosis in Priority order. 1. 2. 3. 154 words <> Insert Table Chart Text Shape Media Comment Collaborate 4. What interventions would you initiate? Independent: Dependent: Describe the wounds? Staging A Staging B Describe . Stage 1 wound Stage 11 Stage 111 Stage 1V Unstageable
(Visited 4 times, 1 visits today)



